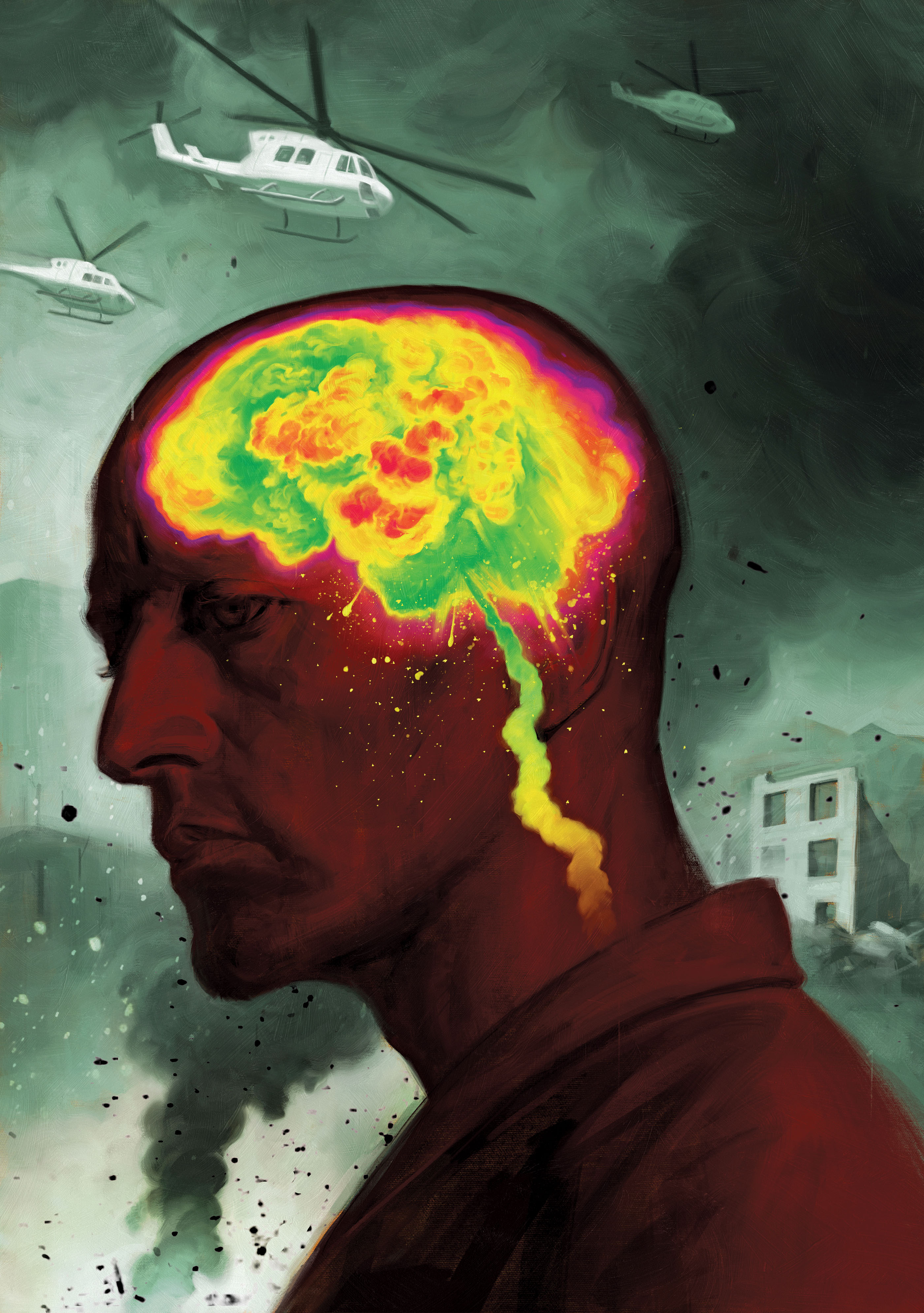
Scanners that show how the brain’s chemistry changes from moment to moment—and from thought to thought—promise new views into the inner workings of the traumatized mind
Retired Master Corporal Don Leonardo of Airdrie, Alta., a third-generation soldier, has battled PTSD since serving with the United Nations protection force in Yugoslavia in 1994, a mission not so much about keeping the peace, but enforcing it at gunpoint.
“There were a hundred incidents,” he says, that contributed to his deteriorating state of mind and growing list of symptoms, including night terrors and a hair-trigger temper. He was diagnosed with post-traumatic stress disorder (PTSD) in 2000.
Leonardo has lived varying degrees of a nightmare ever since. When he would recall his experiences for his psychiatrist, it resurrected past traumas. Over the years, he has been prescribed two dozen different drugs to tackle the night terrors, mood disorders and terrible insomnia. Drugs prescribed to help him sleep left him comatose for 12 hours, his weight ballooned due to a ravenous late-night appetite, and he lived in a fog most of the time. “I felt I was stupid,” he says.
“The treatments themselves are just
not good enough.
We need more tools.”
Sometimes something would work for one symptom, for a while. “And then it didn’t work anymore.” So new drugs were prescribed, one after another. But symptoms persisted: anger, irritability, inability to focus, flashbacks. His life was “a big yo-yo, up and down, getting fired, barely able to get out of bed. I thought, ‘What the fuck is going on? Why am I not normal?’”
PTSD is a tough therapeutic nut to crack. Symptoms vary from person to person. There is no magic bullet, no one treatment, no one drug, no combination of drugs and psychotherapy that works for everyone. Trial and error figures prominently in the search for relief. There are only four evidence-based treatments, and all have side effects that can be so awful that a quarter to a third of patients drop out. For about a third of patients, nothing seems to help much. Some people suffer for years, for decades.
The Canadian Armed Forces has a vested interest in preventing and cutting short that suffering. A study of 792 soldiers who deployed to Afghanistan in 2007 shows that about 25 per cent had developed PTSD within four years and less than 50 per cent had recovered enough to resume their full duties. A 2013 Statistics Canada study finds that five per cent of full-time CAF personnel surveyed had PTSD symptoms—by extrapolation, that’s 3,400 of the 68,000 current full-time serving members. No one knows the number of PTSD veterans, but Veterans Affairs Canada reports about 19,000 of its clients—up from 2,100 in 2002—receive disability benefits for a mental-health condition.
About a third of soldiers with operational stress injuries will improve, a third will still have symptoms but be able to function, and a third will have problems over the long haul, Dr. Jitender Sereen, Professor of Psychiatry, Psychology and Community Health Sciences at the University of Manitoba, told the Senate Subcommittee on Veterans Affairs in 2014.
The CAF wants to do better. “It’s not just us. It’s psychiatry overall,” says Colonel Rakesh Jetly, chief CAF psychiatrist. “The treatments themselves are just not good enough. We need more tools.”
Doctors treating a leg wound can call on solid knowledge of how the bones, muscles, ligaments and blood vessels function together in a normal leg, how different wounds affect function, what treatment can best restore function. And they can track healing with their own eyes. But it’s a different story when something goes awry in the brain.

“The brain is very highly protected. You can’t really get into it, you can’t see it,” says Dr. Zul Merali, president of The Royal’s Institute of Mental Health Research in Ottawa. The brain is the most complex object in the universe. Its billions of cells and dozens of structures operate like a network. Its function is the sum of thousands of complex interactions. When something goes wrong, the whole network can be affected. “You cannot take a slice of the brain under a microscope and begin to understand such complex disorders as depression…and PTSD,” says Merali.
Addressing a mental-health issue is not like setting a broken bone or removing a tumour. Brain function is all about connections—how cells talk to one another and work together.
“In the past, all our discoveries have been post-mortem, after people have passed away,” says Merali. But that is changing. New technology is making it possible to see how a normal brain functions and to learn how that function changes due to illness and injury. And even to track how the brain responds—or doesn’t—to various treatments. “Now we can see inside living brains,” says Merali.
Some of that technology will soon be available for the exclusive use of mental-health research in Ottawa, as the Institute of Mental Health Research unveils its state-of-the-art scanner, which combines positron emission tomography (PET) with functional magnetic resonance imaging (fMRI).
“MRIs tell us where the brain is experiencing a problem,” says Merali, “and the PET lets us figure out what neurochemical change needs to be corrected.” The technology will also be used to advance understanding of how the brain works. “Then you can understand when it breaks down.”
That is good news for veterans such as Leonardo and the thousands of CAF serving members and veterans living with PTSD, depression, anxiety, insomnia and other mental-health disorders.Researchers in military and veteran health are already lining up to use the technology.
The goals for those mental-health researchers, says Jetly, are first to understand the biology of the brain, then to leverage the technology for diagnosis, assessment and treatment.
“And the other big piece is precision medicine or personalizing medicine,” he says—pinpointing the therapies and medications that will work for each individual. Eventually, we’ll be able to celebrate the end of the age of trial-and-error treatment.
The Royal Canadian Legion donated $1 million toward the $7 million purchase of the scanner at The Royal, which is home to a Veterans Affairs Canada operational stress injury clinic and is associated with the Canadian Military and Veterans Mental Health Centre of Excellence, where Jetly holds the Chair of Military Mental Health.
Although dedicated to research, The Royal’s tailor-made scanner holds the promise of a means to objectively diagnose PTSD and other operational stress injuries, shortening the time needed for diagnosis and quelling rumours of faked symptoms. It can tease apart traumatic brain injury, PTSD and its marching buddies depression, anxiety and insomnia. It can be used to show the effect of psychotherapy and drug interventions on the brain, and hopefully one day help determine which combination of drugs and therapies will work for each individual. It might even lead to the means to train the brain to be more resilient to mental injury or even harness the power of the brain’s own network for healing.
But all of that begins with better understanding how the brain works. “Once you know how a healthy brain works,” says Merali, “you can begin to understand what happens when it breaks down.”
“In the past, all our discoveries have been
post-mortem.… Now
we can see inside
living brains.”
Originally developed to diagnose cancer, MRI scanners are now used to diagnose a host of medical problems and extend our knowledge of the body’s structure and how it works. They are even used to produce works of art.
It all began with a eureka moment in 1969, when the Armenian-American physician Raymond Damadian used nuclear magnetic resonance, a tool chemists had used for years, on a bacteria sample, and was stunned by the detailed and instant results.
“I thought if we could do on a human what we just did in that test tube, maybe we could build a scanner that would go over the body to hunt down cancer,” he said in an interview with Inc. Magazine in 2011. More than a billion MRI scans have been done since Damadian perfected his first machine in 1977. Named Indomitable, it now resides at the Smithsonian Institution in Washington, D.C.
MRIs apply a magnetic field tens of thousands of times stronger than the Earth’s own magnetic field to some of the tiniest particles in the human body—subatomic particles in the body’s billions upon billions of atoms.
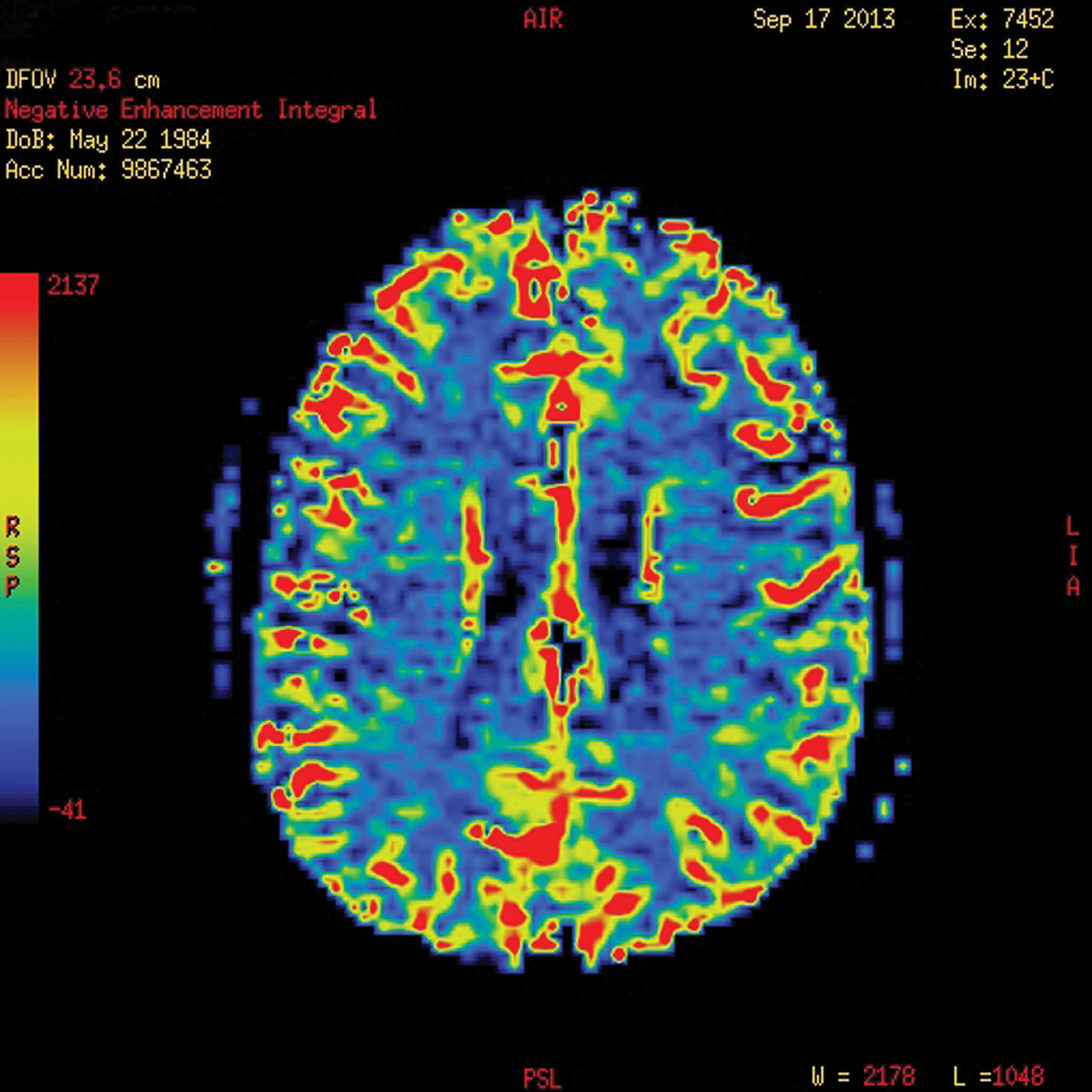
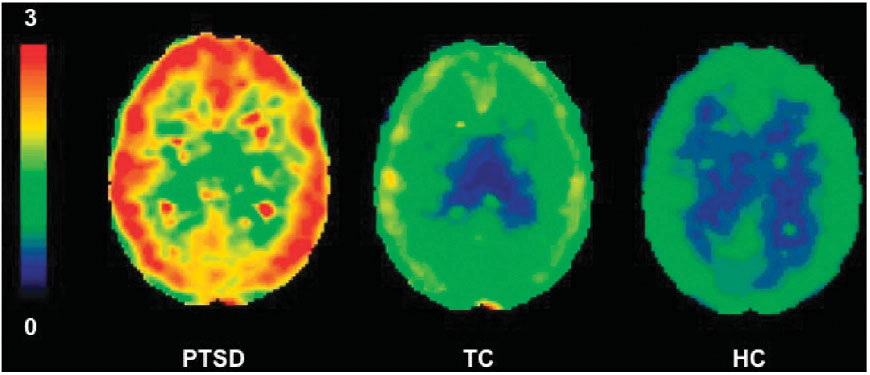
While X-rays, computerized axial tomography (CT) scans and standard MRI scans help researchers see the basic structure of the brain, even more sophisticated imaging is necessary to capture changes in the brain as it works, because brain chemistry can change from one instant to the next. The Royal’s new PET-fMRI scanner marries two sophisticated imaging techniques, and its very powerful computer can combine data from both and produce images of brain activity over time.
An MRI scanner is basically a tube in which patients lie, surrounded by a large, circular magnet, most often a superconducting electromagnet, which is essentially a bunch of wires coiled around a piece of magnetic metal. When electricity passes through the wires, an electrical field is produced. The electric charge encounters resistance from atoms vibrating in the wire, so a large amount of electricity is needed to produce a stable field. Cold dampens the atoms’ vibration, allowing the charge to pass more freely, so the coils in a superconducting electromagnet are held inside a vacuum and bathed in liquid helium at -269°C, and thus much less electricity is required to produce a stable magnetic field.
The MRI’s magnetic field is so strong that it can turn small items like paper clips into dangerous projectiles, and even make oxygen tanks fly across the room. That’s why it is important to inform an MRI technologist if you have an implant or other internal metal object. For example, a bullet or other metallic fragment in your body could change position and cause an injury.
Our blood contains billions of atoms, each sporting tiny electrically charged particles called protons. Protons align in one direction when exposed to the MRI’s magnetic field. Then narrow bands of radio waves in pulses aimed at a certain area knock the protons into a new alignment and cause them to absorb some energy. When the radio waves are turned off, the protons return to their original position, and give off the energy they absorbed as a tiny radio signal. These pulses cause vibration in the machine’s coils, which produces its characteristic thumping sound.
Glucose and oxygen are brain fuel, delivered through the blood. As we think, remember events, react to images, sense touch or hear sound, different areas of the brain go into action, requiring more fuel. Blood flow to those area increases, and glucose and oxygen accumulate.
In oxygen-rich blood, more and stronger radio waves are produced in working areas of the brain. The scanner picks up these signals and transmits that information to the computer, which pinpoints the location of each tiny signal and assigns it a colour based on its intensity.
At the same time, the PET scan detects gamma rays emitted by a tracer attached to another substance, such as a drug used to treat a PTSD symptom, and injected into the bloodstream. More gamma rays are detected where the brain absorbs more of the drug.
The PET information is also relayed to the computer, which combines it with the data from the fMRI. After millions of calculations, the computer assembles these teeny squares of colour into very detailed pictures of wafer-thin layers. Like a loaf of sliced bread, these pictures can be “stacked” into three-dimensional images. The harder working areas of the brain stand out from surrounding tissue, and researchers can see changes over time.
Eventually,
we’ll be able to
celebrate the
end of the age
of trial-and-error treatment.
Although relatively new technology, it has already made significant contributions to our knowledge of the brain and how it works. One U.S. study showed that activity in one area of the brain predicts whether a depressed person will react better to cognitive behaviour therapy or an antidepressant. Others have found that PTSD not only alters the brain’s chemistry, but its function and structure as well. It has also revealed differences in brains affected by PTSD versus traumatic brain injury.
It has even been used to tease apart fine emotional distinctions: people with furry companions often refer to themselves as pet parents, but scans reveal that mothers’ brains react differently to their children than to their beloved pets.
Leonardo has not had much luck with evidence-based PTSD treatments, and he worries about how such new technology as PET-fMRI scanning might be misused. But, he says, “I’m all for them being able to see what’s going on in the brain.”
On his own, he has found some relief through hypnosis, tried service dogs, turned to God. He discovered he could help himself by helping others, including establishing the online social-networking community, Veterans of Canada. Now he is seeing a psychologist and is off all medications except sleeping pills, which help him get a meagre four hours or so a night. “I am starting to wonder if anything will help. You learn to live with what you have.”
If this new technology lives up to its promise, perhaps one day Leonardo will be prescribed treatments that quell, rather than mask, his symptoms. Maybe then he will finally get a good night’s sleep.
Advertisement