With this issue, we begin a new column called Military Health Matters. Health advice columns, news on civilian health research and analysis of public health issues abound in newspapers, magazines, blogs and websites—but much less is available on issues concerning serving military, veterans and their families.
Yet military health research and development greatly benefits society—and not only those in uniform or those who care for the people who wear or wore them. The public also benefits from new techniques and treatments discovered and developed for military use.
Military and veterans’ health is a public health issue as well. We all benefit when our military members receive better care while serving so that they enjoy better health as veterans. Healthier veterans are more able to contribute to their communities and their health care becomes a smaller burden on society’s resources.
We can only imagine what a difference it would have made if, after the Second World War, there had been enough knowledge and money to treat every soldier with post-traumatic stress disorder. How much family violence, how many cases of addiction, how many suicides and wrecked lives would have been avoided?
Many societies have come to realize it is cheaper to prevent problems, treat them early, and use treatments and therapies that are proven to work. Countries around the globe are investing in research institutes and establishing research networks to tap into expertise at universities, private industry and the military itself.
Health problems are common to military personnel regardless of what country they serve—yet there are differences country to country in prevalence and treatment. For instance, researchers at King’s Centre for Military Research and the Academic Centre for Defence Mental Health in England documented that post-traumatic stress disorder is lower among British than American troops. Could the two countries be counting cases differently? Or could the differences be linked to Britain’s shorter deployments, higher officer/troops ratio, training differences or the use of decompression after deployment?
At home, we benefit from research done by the Canadian Armed Forces, the Canadian Institute for Military and Veteran Health Research, Defence Research and Development Canada (DRDC), and the veterans and military ombudsmen strengthened by hundreds of researchers at universities and in the private sector. Following are just a couple of examples of recent research.
Hearing loss is not uncommon in professions requiring gun and artillery practice and use. Veterans Affairs Canada pays about $180 million a year for hearing-loss benefits, disability awards, services and hearing aids. DRDC researcher Ann Nakashima at the Toronto Research Centre compared a number of hearing-protection devices, ear plugs and ear muffs that can be used during weapons firing. Her data can help people choose the device for each job that strikes the right balance of protection against damaging sound levels during firing and requirements for communication and background noise. Her work was presented in part at the 2014 Military and Veterans Health Research Forum.
The feasibility of providing periodic health assessments to primary reservists was the subject of recent research released by the military ombudsman and the Canadian Forces Health Services Group. Reservists must also meet the Canadian Armed Forces’ universality of service requirements, which mandates military personnel be employable and deployable, with a medical assessment to prove it. Regular force members can get these assessments through CAF Health Services. Reservists cannot.
Veterans Affairs Canada pays
about $180 million a year for
hearing-loss benefits, disability
awards, services and hearing aids.
A quarter of Canada’s 26,777 primary reservists do not have a current assessment on file. Although they are eligible for some CAF health services for service-related injury and illness under particular circumstances, reservists must mostly rely on the public health services of their home provinces. Yet nearly 40 per cent of reservists do not have a family physician, the report notes.
Lacking a medical assessment could complicate a reservist’s legitimate future claims for service-related compensation and benefits as well as open the door for fraudulent claims, the report says. Anyone reading the report must wonder how, without the assessments, are commanding officers to know if their reservists are fit to be employed or deployed? How are service-related health problems to be spotted?
While the medical needs of regular forces are managed by CAF Health Services, the report said, rules for reservists are so vague that “a considerable amount of healthcare providers’ time is devoted to determining entitlements.” The regulations governing medical services were last updated in 1985; reservists have deployed in 27 overseas operations since 1994, and 8,000 have been involved in domestic operations since 1997. Reservists made up between 15 and 25 per cent of rotations to Afghanistan.
Now is a good time to consider this question, as the role of the reserve force is currently under review, medical services regulations are being updated, and the CAF is reviewing how often health assessments should be done.
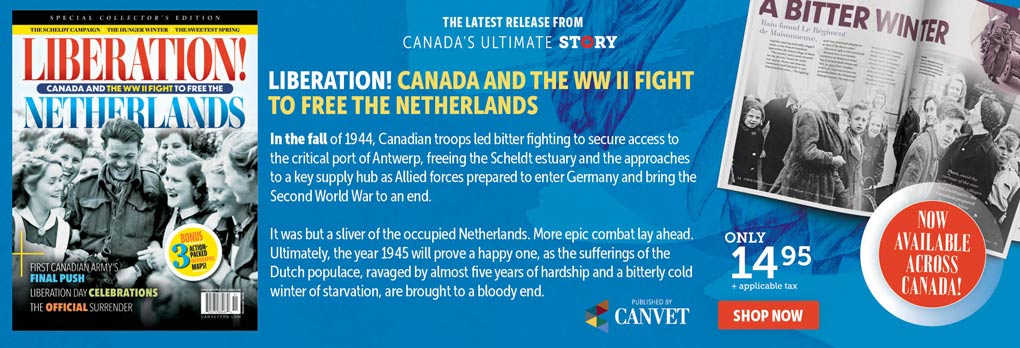
Advertisement