The question is: What, in your view, is preventing the treatment of veterans with PTSD in Canada?
Retired Lieutenant-Colonel Chris Linford, author of the new book Warrior Rising: A Soldier’s Journey To PTSD And Back, leads off with what we hope will be a meaningful, online discussion, involving other veterans, their families, health care professionals and those conducting research on the topic.
Here’s what Chris Linford had to say:
“This is the million-dollar question as the government and Canadians at large thirst for an understanding of PTSD, and try to answer what is the right level of support needed for injured Canadian veterans.
“The fact remains that it is often the veteran who is the major barrier to accessing clinical treatment!
“From a personal perspective, it was something I struggled with for years when impacted by PTSD after my deployment to Rwanda. Due to stigma, both self-imposed and societal, I put off sourcing help until my injury became so severe, I had to reach out and was finally diagnosed with PTSD and depression 10 years after the fact.
“In short, the stigma concerning mental health issues in my mind prevented me from sourcing the care I needed.
“I was my own worst enemy!
“The help may have been available to me but I had no interest in any of it until I could cope no further and had to do something. It was when I hit the very bottom of my health when I finally realized I would need the help of the Canadian Forces Health Services as well as my community to realize good health again. I felt weak and judged, thinking I would be rejected by my peers; I was wrong. My poor understanding of PTSD and continued self-stigmatization fed directly into my inability to find true healing over the years. So why was I like this?
“It is very much part of the soldiering culture that makes it against our nature to identify ourselves as injured. This mindset is inculcated from the first day of basic training as military directing staff attempted to make soldiers out of a bunch of snotty nosed civilians.
“The intent was to make us hard and if required, willingly lay down our lives for each other and Canada. It made perfect sense to do this given what we trained to do; fight our nation’s wars. To be injured or rendered incapable of fighting or doing our job was a place most of us would never purposely envision for ourselves. I fully participated in this culture and for years felt no particular compassion or patience for anyone I had to remove from the order of battle due to illness or injury.
“Regretfully, my attitude as a leader was harmful as I was focused upon the current mission; I never recognized PTSD as an injury and thus had even less understanding and compassion for myself when I became impacted. Any sort of inability to cope with the stresses of the mission were not entertained or tolerated. From this we all learned early in our military careers that self-sacrifice is expected and in fact highly encouraged. This is a critical aspect of the military mindset and should be sustained to ensure initial mission success, but if we continue to think only in the short term, we must also accept that it will be difficult to get our soldiers with injuries to step forward early when management would/could be easier.
“Years after my deployment to Rwanda, I began to notice the changes in myself. I had already witnessed a significant rise in the number of PTSD casualties from my unit during the year after this highly emotional and traumatizing deployment. I found myself vigilant and guarding how I acted around others who could potentially discover I was injured.
“I did my very best to hide my injury and essentially dismissed any thoughts that I might be less than capable of doing my job; I was fearful of losing my military career, something I held in the highest regard. I would not lose that at any price!
“The interesting thing about that way of thinking was that it didn’t take into consideration getting help before the injury worsened. Imagine if we thought that way about a bad cut on our foot. It wouldn’t be long before things would turn ugly and the next thing you know we would be in a wheelchair.
“So what makes a stress injury so different?
“I believe it has everything to do with the fact that it is invisible and also that it is a mental health issue. PTSD has been referred to as an invisible injury at many levels but in fact if one pays attention to the behaviour of someone who suddenly after a deployment becomes indifferent, withdrawn, quick to temper and seems to not enjoy the things he/she used to; one might consider these are symptoms almost shouting out to be attended to!
“Mental health illness in our society has long been considered one of those things we just didn’t talk about. Many of us have at least one family member who over the years has been mentally unwell and the rest of the family simply made excuses for them or ignored them all together. This common and stereotypical action has made it extra hard for highly trained veterans to do their jobs under the most arduous of circumstances to even begin to consider stepping forward and identifying themselves as having such an affliction.
“In speaking with veterans suffering with PTSD, depression and other anxiety issues, a statement I frequently heard from them was that they felt they were not “worthy” to receive help. They would compare their injury to those of other “more deserving veterans” who really had it bad. This martyrdom approach, although impressive, seemed to be more prevalent among the senior non-commissioned and commissioned ranks. If allowed to continue it will serve to allow a dramatically worsened problem in the future among this group. All veterans deserve and are worthy of living life with health no matter what their war experience was!
“From the bigger picture and perspective, what is preventing veterans with PTSD from getting care? Is the Canadian Government responsible to be the total answer with this one?
“My personal perspective is that Canadian Armed Forces personnel are sent on deployments on behalf of all Canadians where we are sometimes confronted with significantly violent events and stressors that can lead to injuries and/or death. To be clear, I make no delineation between physical and mental health injuries. Therefore I believe that on behalf of all Canadians, the Canadian Government, Canadian Armed Forces chain of command, and Veterans Affairs Canada are ethically and morally obligated to try and return injured veterans to good health and compensate them appropriately.
“Having said that, veterans should not expect a “free lunch” in the form of “any and all” unproven resources and compensation; the answer is not that easy. The commitment to improving an injured veteran to the best possible health must be the prime driver. I believe there needs to be a solid partnership between the military, government and the injured veteran to see this through to success.
“An injured veteran is best to ask for clinical intervention while still serving in the Canadian Armed Forces. In my view, the current infrastructure that is in place from coast to coast is better than anything found exterior to the military. The challenges have been significant for Canadian Forces Health Services to meet the demand as not all military base locations can support the need. CFB Petawawa has been in the news lately regarding its capacity to manage veterans with stress injuries. Given the base’s location about two hours west of Ottawa, it has been difficult to hire mental health clinicians in enough quantity to manage the population of injured veterans and their families. As a result, CF Health Services has been able to reposition uniformed clinical staff there as well as bolster the relationship with non-clinical resources to further reduce wait times and ensure a more holistic approach to care is taken. I do fear it will take time to change opinions on the level of care available in Petawawa, perhaps an education plan is required to best inform of the changes implemented.
“Every injured veteran deserves access to good clinical care for any wound and especially those sustained during deployed operations. This may mean he/she must travel, taking them away from the stability of the home and family. This can become hard to manage especially for injured veterans suffering with PTSD. More must be done to get well trained clinical staff to the injured veterans. It should not be the other way around.
“When a veteran leaves the military without a diagnosis of PTSD and is later found to have PTSD through assessment, they will find a dramatic difference with what is available for them through provincial health care and Veterans Affairs Canada (VAC). There are many excellent clinicians across the country working in private practice as well as clinics that can help veterans with PTSD, but many are unfamiliar with the context surrounding a PTSD contracted through combat operations. Injured veterans have frequently stated that often these clinical specialists have difficulty understanding their circumstances and thus have difficulty building the much needed relationship of trust with that clinician.
“I believe the one group of injured veterans at the greatest risk of not getting the care they need for their PTSD is the Canadian Reservists. This group of young men and women who willingly chose to put their civilian lives on hold to deploy and serve Canada have returned home to sometimes fall between the cracks when it comes to medical follow-up. Many have returned to units who can quickly lose track of them as it is not a requirement for them to show up consistently. It can be weeks and months before they are seen and maybe never at all. Their family physician is often not versed in PTSD or able to relate to the combat context the veteran presents with and thus the frustration and disillusionment builds within that young reservist leaving them feeling isolated and abandoned.
“It should be known that any reservist with a deployment history can present themselves to any Regular Force Medical Unit and be assessed for injury and if they are found to have a deployment related injury, they are entitled to care paid at Crown expense. I have discovered that many reservists are unaware of this policy.
“At times and due to the distances between some reserve units and regular force medical units, to get care, injured veterans must travel that distance often causing significant complications to an already stressed situation. At times I have no doubt that this situation alone has prevented injured veterans from even sourcing the assessment and eventual care. Instead they would just learn to live with or cope with their injury at great personal cost. This group of Canadians are perhaps the group at greatest risk of a worsening PTSD leading to continued poor quality of life and potentially greater risk of suicide.
“Even though there is a much improved understanding of PTSD across Canada; there is a lot of work left to do. I believe the only way to truly reduce barriers to accessing care for veterans with PTSD is to ensure that education continues along with an honest conversation regarding this injury.
“If this takes place and we as a society continue to have this candid discussion, we may in the near future even forget that this injury was ever stigmatized. Veterans and their families will then fully understand the need to come forward early to get help. Injured reservists will feel empowered to come forward for assessment even after their missions are long over and be assessed for needed care. The government will know that early intervention is needed and respond by ensuring our veterans have what they need to return to fruitful and healthy lives. It all starts with a candid and honest conversation but it will take the combined efforts of the individual veteran and the government and CAF to dramatically remove all barriers to receiving the care needed for PTSD.”
Our goal with The Veterans’ Hotwash is to create an active online discussion on the question Chris has just answered, and on other questions that will follow.
We encourage you to participate in this blog by submitting a blog post and by commenting on what Chris had to say. Do you agree or disagree? What do you think is preventing the proper care of PTSD veterans in Canada? What else can or should be done? We would really like to hear from you.
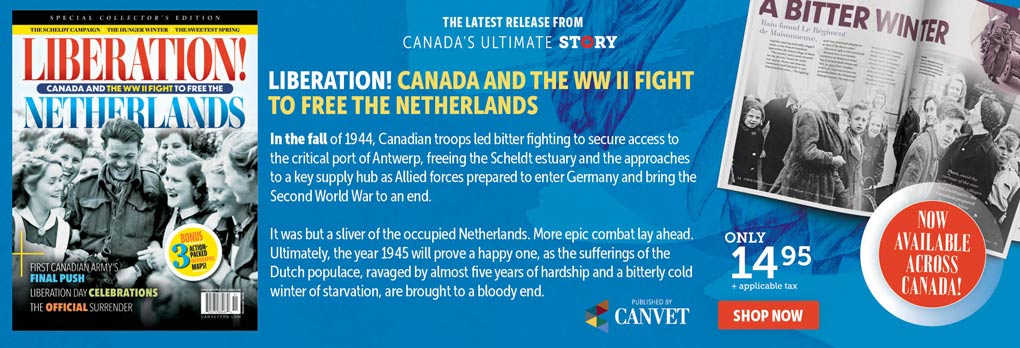
Advertisement
No related posts.