Insomnia and pain are big problems for both serving military and veterans. Years of rotations, long and alert hours, frequent travel and skipping across time zones can disrupt sleep cycles, can turn the odd sleepless night to the burden of insomnia. Post-traumatic stress disorder (PTSD) and traumatic brain injury (TBI) can make that burden unbearable. As well, the physical nature of the work results in injuries and wears down joints, and can result in chronic pain.
Resolving these problems can be a long, drawn-out battle. Often military personnel first turn to alcohol and recreational drugs, which can temporarily help them log more zzzs or dull the pain, then move on to medical treatment which often involves prescription drugs with unpleasant side-effects.
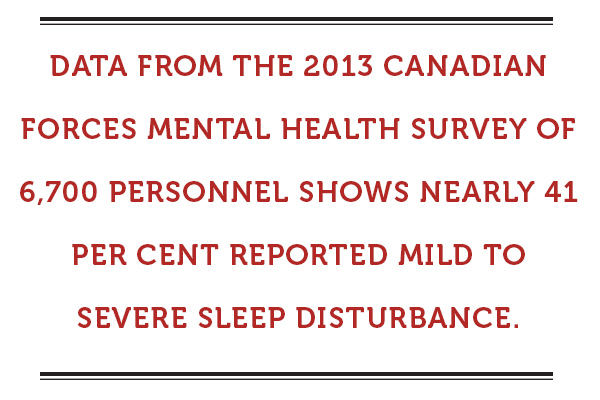
Data from the 2013 Canadian Forces Mental Health Survey of 6,700 personnel shows nearly 41 per cent reported mild to severe sleep disturbance. It also indicates a relationship between sleep disturbance and thoughts of suicide.
U.S. military research found members with insomnia prior to deployment were at higher risk of developing PTSD, depression and anxiety after combat. It also found that 44 per cent of those deployed develop chronic pain (compared to a quarter of the general population). And that chronic pain can affect and be affected by lack of sleep.
The U.S. military is investing in dozens of studies of non-drug means to manage pain and sleeplessness.
One is investigating harnessing the brain’s own power to promote sleep.
Brain cells communicate electrically, the millions of “chatting” neurons producing synchronized pulses—the “brainwaves” so familiar from television medical dramas. The complex interaction is like music, with certain mental states producing characteristic patterns which can be picked out, like focusing on the strings or horns in an orchestral performance. When the soundtrack of the brain is reproduced visually, sharp peaks and valleys generally indicate wakefulness, with waves getting longer and flatter as we fall asleep and move into deep sleep.
The brain can be coaxed to alter wave patterns to match the rhythm of flashing lights or the beat of music (perhaps explaining why we can put infants to sleep with lullabies and massage therapists can put us into Zen-like relaxation with soothing music).
Now biotech companies are developing devices to aid this process. The U.S. Army Research Office has invested in the research of Brain State Technologies in Arizona, in conjunction with several medical schools, that has resulted in a wearable sleep aid.
The device looks something like a plastic headband young girls use to keep long hair out of their faces, only worn across the forehead. Sensors in the band pick up brainwaves and software translates the midrange frequencies into sounds of varying pitch and rhythm, which are played back to the wearer through earbuds—brain music, if you will. The brain adjusts to mirror the rhythm, altered brainwaves setting the stage for stress release, improved sleep and restored circadian rhythm.
The company, whose careful disclaimers point out the device is “not intended to treat, cure, heal or diagnose,” says clinical trials have shown better sleep among military personnel who’ve used the device engaged in “office” duties (presumably not on, or in preparation for, deployment). There are few real-life reviews as yet.
Moving from sound to light, a number of veterans with lower back pain have been recruited for a study at Rush University Medical Center in Chicago using light therapy to quell sleep problems and, hopefully, manage pain.
Our body clock, known as the circadian rhythm, is tied to the light cycles in our 24-hour day. Shift work, travel across time zones and screen time all interfere with release of brain chemicals that control the sleep/wake cycle.
Light therapy is not new—it’s been used for treatment of seasonal affective disorder for years. It’s known exposure to bright light (usually in the morning) restores the circadian rhythm, promoting better sleep. But this research will help determine if better sleep helps reduce pain, and if so, how much, as well as how long veterans need to be exposed to bright light to affect sleep and pain, and how long the effects last.
And, no doubt, it will result in development of new devices and/or treatment protocols.
Many tech companies are on this bandwagon, developing devices to monitor sleep, brainwaves, physical condition, stress, fatigue, and on and on. Some are based on pseudoscience and slick marketing, as opposed to research evidence. And these devices—legit or otherwise—carry a price tag hefty enough to induce sticker shock (Brain State’s device is more than US $1,000).
For benefit plans shelling out thousands of dollars yearly to cover pain and sleep medications, investing in a legit device could be a bargain. But until the military starts using a particular brand, which product is legit? And desperate people in the throes of insomnia or wrestling with chronic pain are willing to pay any price for relief, making them good targets for slick marketers promising relief only a mouse-click away.
Advertisement