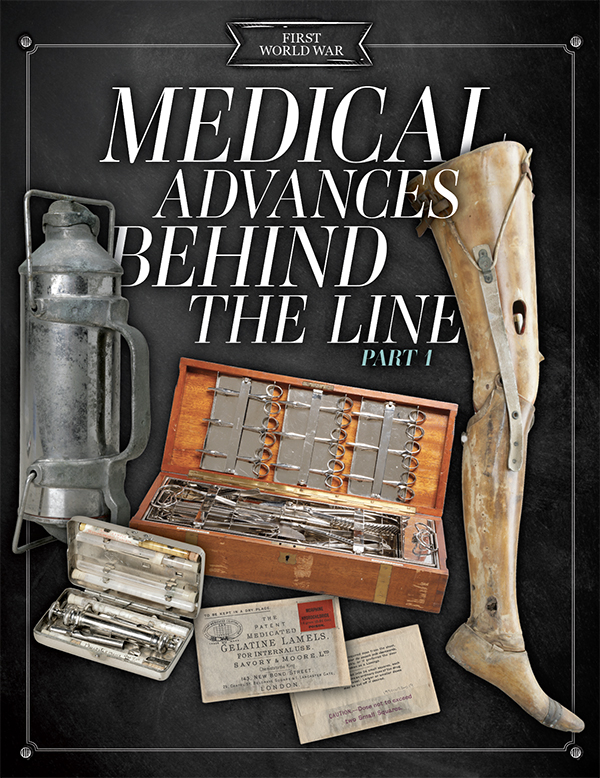
The First World War spurred medical innovations that have since saved countless lives.
In a war of attrition, where huge armies met in battles that could go on for months, keeping the men fit to fight required as much thought and effort as battle preparations.
While the military war was waged in intermittent battles against the enemy across no man’s land, the medical war was an endless fight against mites and microbes and horrific bodily damage wrought by the mass killing machines of the First World War. Victory on both fronts required medical breakthroughs.

A soldier picks lice from the seams of his shirt in 1918. The parasite transmits bacteria that causes fever, headache, leg pain and sore eyes. It came to be known as trench fever. [CWM/19900073-019]
Men, mites and microbes
“Well! I don’t know which is the worst. The war or the lice.… When we are in the trenches, what little time we get to sleep, the lice won’t let us.”
—Samuel Warren Ball, April 1917 (from the Canadian Letters and Images Project)
Throughout history, more troops have died from disease than combat. More than half of Canadian troops who died in the Boer War succumbed to germs, not guns.
But less than 10 per cent of Canadian First World War troop fatalities were attributed to disease—rather astonishing, considering the filthiness of trench warfare. Muddy trenches and shell craters were cesspools contaminated by garbage, human waste and rotting corpses—ideal breeding grounds for diseases as well as the rats, lice, flies and fleas that spread them.
What made the difference? In the First World War, high command took prevention seriously, beefing up the medical service and making officers responsible for hygiene and sanitation in their units.
The more than 16,000 Canadian medical personnel overseas included experts in infectious disease, water purification and bacterial disease, supported by a mobile laboratory. The medical corps had sanitary sections that conducted regular inspections to ensure standards were followed.

“I have my daily sanitary inspection of all the camps, and then have my sick parade.”
—Dr. Charles Willoughby, Sept. 2, 1918
Cleanliness was a never-ending battle but produced many victories.
“A war without dysentery is one of the strangest phenomena of military record; and yet Canadian medical officers served for their whole time on the Western Front and never saw a case,” wrote Sir Andrew Macphail in the Official History of the Canadian Forces in the Great War: The Medical Services.
Ensuring supplies of clean water and food and sanitary disposal, disinfection or—far better, burning—of refuse and human waste were one key to disease prevention. Vaccination was another.
In 1914, 32 per cent of the British wounded contracted tetanus. Dr. John FitzGerald, who had established an antitoxin laboratory at the University of Toronto, was asked to produce enough vaccine to inoculate every Canadian soldier.
Troops at the front were inoculated against typhoid, tetanus, smallpox, cholera, diphtheria and meningitis.

A soldier is vaccinated at CFB Valcartier in Quebec, c. 1914-15. [Bain News Service/U.S. Library of Congress/2014697179]
Letters from the front familiarized the civilian population with the effectiveness of vaccination, which remains a cornerstone of public health.
“It certainly looked bad. Some of the fellows…turned white and many fainted away. I guess it bothered me less than it did most.… I hardly felt it at all.”
—Robert Gordon Brown, Jan. 23, 1916
Unwashed bodies and clothing provided homes for unfamiliar microbial foes that proliferated in the mucky environment. A new kind of jaundice was traced to bacteria in human and rat urine. About 10,000 troops suffered from scabies, a contagious skin disease caused by mites. Trench foot, arising from tissue damage from feet continually wet for days, afflicted at least 5,000, and at least the same number were treated for trench fever, a mysterious condition that affected the spleen and caused long-lasting fatigue. It was eventually traced to lice and an eradication campaign followed. Around 10,000 troops suffered from trench mouth each year.
“They gave out whale oil for our feet to prevent trench foot. Most of the men got it and rubbed it on their feet making them a beautiful mahogany brown. Afterwards it was found that they had got the wrong stuff and they had been given lice killer.”
—Henry Crozier Smith, Oct. 28, 1916
Disinfection centres had bathing and laundry facilities but men returned to lousy environments and were quickly re-infected. Individual use of disinfectants and meticulous manual delousing of body and clothing continued right to the end of the war.
“The lice killer you sent me did the job all right! I had about 500 of them and can only find a few now. One tin a month will be enough to send out to me.”
—Arthur Calvin Smith, June 19, 1917
Lives of the wounded also depended on the battle against microbes. To medical officers at the front, “all wounds were infected,” wrote McPhail. A French surgeon said in 1915 that 70 per cent of amputations were due to infection.
The widespread use of antibiotics, such as sulfa drugs and penicillin, was still decades in the future. Wounds were treated with a variety of antiseptic substances “but were of most value in wounds that would have healed without them.”
Iodine was the favourite, but flavines, boric acid and even salt were used. “The solution of hypochloride of lime was also a favourite. When it was poured into an open wound, bubbles of gas could be seen arising, and gave off the wholesome cleanly smell of diluted chlorine,” wrote Macphail, who served at the front in a field ambulance unit.
“Happily my feet are not sore, the boracic powder with which I filled my socks prevented that.”
—Albert Feredey, June 8, 1918
By the end of the war, Allied doctors had adopted a method of wound sterilization developed by British biochemist Henry Dakin and Nobel Prize-winning French physician Alexis Carrel. Carrel invented the irrigation system through which a wound was regularly flooded with a sodium chlorite antiseptic solution developed by Dakin. The incidence of gas gangrene decreased, and with it, the need for amputating limbs. A Dakin solution is used to this day to kill germs and prevent their growth in wounds.
Broken bones and X-rays
Early in the war, 80 per cent of those who suffered a broken thigh bone died, half in transit before reaching a field hospital. Broken ends of bone moved and grated, severing blood vessels and causing horrendous pain; troops died of blood loss and shock. Knowing the risk, surgeons often amputated, rather than trying to save the leg.

A surgeon, assistants and a nurse operate on a patient in No. 10 Casualty Clearing Station in France in July 1916. [Henry Edward Knobel/DND/LAC/3395769]
Welsh orthopedic surgeon Robert Jones introduced the use of splints on the battlefield. [Wikimedia]
It was first used by Canadians at Vimy Ridge, but by the end of the war, there “was a splint ingeniously modified for every form of fracture.” Thomas splints are still used today.
The splint was often used in concert with another innovation that gained acceptance during the war and is now in regular use in Canadian hospitals—the X-ray machine.
The Canadian medical service was supplied with more than 500 X-ray units and used more than a million X-ray plates a year.
Nobel Prize-winning French physicist Marie Curie could see the benefit of X-rays in treating the wounded, but the machines were exclusively hospital equipment in 1914. She directed the outfitting of vehicles with X-ray machines and darkroom equipment—they could drive right up to the battlefield. She was also instrumental in the construction of more than 200 radiological rooms at field hospitals near the battle lines.
X-ray apparatus allowed for “corrections [that] could be made by bandages, pressure or extension to secure a perfect alignment” of broken bones, wrote Macphail. They were also used to follow the progress of healing fractures and by surgeons to locate bullets and shrapnel for removal.
“It was a machine-gun bullet in my left thigh, about four inches above the knee…. The bullet was located by the X-ray and early in the afternoon I went to the operating theatre where the offending missile was extracted.”
—Frank Cousins, Sept. 1, 1918

Medics tend to the wounded in a trench near Courcelette, France, in September 1916. [William Ivor Castle/DND/LAC/PA-000627]
Banking on blood
Mechanized butchery made the First World War the bloodiest in history. In the Battle of the Somme alone in 1916, there were more than a million casualties, including more than 24,000 Canadians and Newfoundlanders.
In addition to bleeding out, blood loss caused death from shock.
The standard British treatment, a saline infusion to bring up the fluid level, did little to stabilize shock. But Canadian doctor Bruce Robertson, who had trained in new transfusion technology developed in the United States, was able to persuade colleagues that transfusion of whole blood was better for treating battlefield wounds.
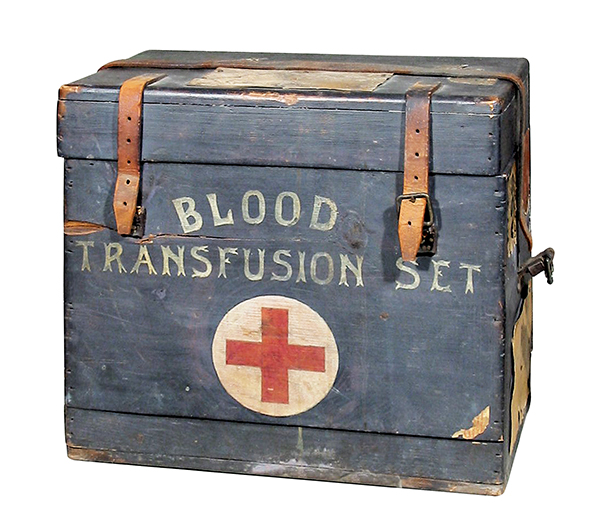
A portable blood-transfusion kit belonging to Canadian doctor Norman Miles Guiou. He was a pioneer of blood transfusion, an important evolution in combat surgery. [CWM/19980102-003]
But ironing out the wrinkles in this new technique took some time. Donated blood clotted so readily that it could not be stored. Canadian Major Edward Archibald pioneered the use of sodium citrate as an anticoagulant as early as 1915, according to Canadian Blood Services, but the credit was given to Captain Oswald Hope Robertson, a medical officer with the U.S. Army Medical Corps.
The importance of cross-matching blood type slowly became understood. Donors lined up for person-to-person donations until Robertson came up with the idea of storing blood for later use. He used only Group O blood because it is compatible with all other blood types. By the end of the war, medics carried standardized kits to perform transfusions in the field.
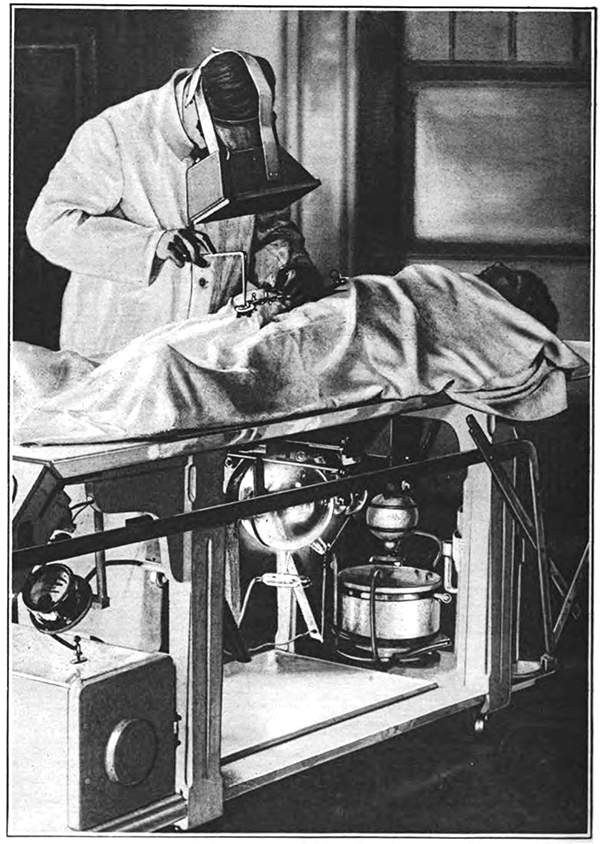
A surgeon wears a fluoroscope to locate bullets in a wounded soldier in 1917. An X-ray tube under the table emits a beam of X-rays vertically through the patient’s body and bullets appear in black on the fluoroscope screen. [J.P. Hoguet/Wikimedia]
—William McKee, Sept. 20, 1918
Transfusions became practical during the war, and after the war they became a regular feature of medical care. The first permanent blood banks were established in the 1930s, and today, making a regular donation to Canadian Blood Services is part of many civilians’ lives.
Painless surgery
“Going into oblivion under the ether and returning to consciousness are strange sensations difficult to describe.”
—Frank Cousins, Sept. 5, 1918

Within an hour of being wounded, a soldier is operated on in a Canadian Field Ambulance in October 1916. [William Ivor Castle/DND/LAC/3395819]
There was no guarantee that the person administering anesthesia had any training to do so, anesthetic agents were not standardized, and there was little specialized equipment. Also, dripping anesthetic onto an open mask released anesthetic vapours into the operating room, where it was inhaled by medical staff.
All of which made anesthesia dicey. Too little anesthesia gas and the patient woke up; too much and the patient turned blue from lack of oxygen. Many patients in shock died on the operating table.
That would change over the course of the war due to the introduction of less-toxic anesthetics derived from morphine, safer and more reliable methods for administering gas, and recognition that one size does not fit all when it comes to anesthesia.
The war, with its great number of wounded and injured, cut short the time needed to determine which anesthetics worked best on which patients and under what conditions.
Captain Geoffrey Marshall, a British medical officer, developed a gas/oxygen mixture that was credited with reducing the surgical mortality rate.
Francis Shipway invented an apparatus that could deliver warm anesthetic vapour directly into a patient’s lungs through an intra-tracheal tube or to a wire-frame mask sheathed in gauze.
This method conserved 60 per cent of ether at his casualty clearing station, Marshall noted, and there was less diffusion into the operating theatre, “an important consideration,” he said, “to those working in it.”
Marshall’s research established that the best results came from tailoring anesthesia to the patient’s condition. For instance, he observed administering spinal anesthesia to a patient who had recently lost a lot of blood caused a serious lowering of blood pressure. “It is important…to recognize beforehand which cases will tolerate this procedure,” he said.
In 1918, it was decreed that each casualty clearing station should have at least one expert anesthetist. It was an important step toward the development of anesthesiology as a specialty.
With more time to work, surgeons could tackle more complex operations and save more lives and limbs. They now had time to find shrapnel in an abdominal wound, to remove all the bone splinters from shattered limbs, to attend to a patient’s multiple wounds in one session.
Improvements in anesthetics spurred development of new surgical techniques, such as bone and skin grafts, and the growth of new medical specialties, such as orthopedics, which focuses on the musculoskeletal system. Plastic surgery, a familiar specialty today, grew from facial reconstructive surgery, which provided men whose faces had been mutilated with better function and a more normal appearance to ease return to civilian life.
Casualty evacuation and triage
Today we think of an ambulance as a vehicle but during the First World War they were known to be mobile medical units.
“A field ambulance being a completely mobile unit which moves with the front line and operates immediately behind it on advance or retreat,” wrote Macphail. Each field ambulance served—and moved with—one infantry brigade. It was made up of regimental aid posts on the front line, advanced dressing stations, main dressing stations and casualty clearing stations.

A horse-drawn ambulance picks up wounded at an advanced dressing station near the front during the Battle of Flers-Courcelette on Sept. 15, 1916. [William Ivor Castle/DND/LAC/3194276]
“An ambulance consists of three or four different stations,” Dr. Charles Willoughby wrote in a letter to his family in 1918, explaining his rotation through transport lines, the main dressing station, the advanced dressing station and the division collecting post.
“At present we are ‘in the line ambulance,’” but, he reassured his family, “one to three miles behind. So don’t start and think we are holding any front line trenches. Nothing of the kind.”
Transport division drivers moved the wounded in horse-drawn or motor ambulances, some of which had been donated by civilians.
“To the end, horse ambulances had quite definite uses,” wrote Macphail. “They had access to areas impossible for motor transport where roads did not exist, readily evading shell holes and making detours into fields.” They were also less damaged and more readily righted if they tipped over.
But they could be brutal on the wounded. On Jan. 27, 1917, the war ended for Harry Morris. A shell explosion split his knee joint and fractured his thigh bone. After a long wait, he was loaded into a horse ambulance that crossed a battleground full of shell holes.
“Every jerk goes through my leg like a knife,” he wrote to his family in April 1917. The transfer to motor ambulance was “a relief for my leg.… As I am being put in, I notice by aid of the stretcher-bearer’s lamp the following words: ‘Presented by the Children of Nova Scotia, Canada.’”
Morris was operated on at a casualty clearing station and remained there until it was safe for him to be moved by train to a Canadian General Hospital, where his wound was tended. A few days later, he was sent to a convalescent hospital in England.
Often the field ambulance transport system was overwhelmed by the sheer number of wounded. Then a motor-ambulance convoy was required. Convoys had 50 cars, a workshop for repairs and more than 100 staff to convey patients from dressing stations to a casualty clearing station kilometres away.
Macphail reported that 48 had been mobilized by war’s end, “coming literally in hundreds of cars apparently from nowhere and clearing the most crowded front in a space of time that was measured in minutes.”
Men were sorted at field ambulance stations in a process known as triage. Those with slight wounds were treated quickly at dressing stations and sent back to fight; others moved up the line, to be treated in order of severity. Those too far gone to save were made as comfortable as possible while medical staff concentrated on the severely injured who might be saved. Those with injuries that were not life-threatening had to wait their turn.

Ambulances with the 3rd Canadian Field Ambulance stand ready to roll in July 1916. [Henry Edward Knobel/DND/LAC/3194237]
By the end of the war, the Canadian Army Medical Corps was operating 16 general, 10 stationary, seven special and eight convalescent hospitals, which handled 539,690 cases, “of which 144,606 were casualties in battle,” wrote Macphail.
But millions have since benefited from knowledge brought back to Canada by doctors and nurses who built on that knowledge and continued to innovate when they resumed their civilian careers.
Advertisement