The epic struggle to understand
and treat the damaged brain takes
place both at the frontiers of science
and in the pharmaceutical Stone Age
In April 19, 2006, Aaron Bedard’s brain changed forever.
That day the Princess Patricia’s Canadian Light Infantry combat engineer and five comrades were in a vehicle that drove over and detonated an anti-tank mine in Afghanistan. “My head was about six feet away from the point of detonation. My neck was rocked violently forward. I got a severe whiplash.”
At first Bedard thought he was lucky. The others suffered serious back injuries and ruptured ear drums and were medevaced back to Kandahar. But Bedard’s injury was invisible. “It was a typical ‘suck it up, soldier’ thing. I looked at myself and I don’t have a scratch on me and if I had said, ‘Oh, yeah, I’m hurt. I’m going to get on that helicopter and go back,’ I’d look like a faker and I didn’t want that. So I carried on.
“I took some painkillers and got on with the tour. I told them I had a really bad headache, but I’d be fine.”
He was anything but fine.
Explosions deliver a double whammy to the brain. First there’s the damage associated with any serious vehicle wreck. As soldiers’ bodies are thrown and jolted, their heads, weighted down by helmets, accelerate forward and jerk back, their brains sloshing around in their skulls like Jell-O in a container dropped on the floor. The brain bangs into the skull in one direction, then bounces back to hit the opposite side. The various layers—the cerebrospinal fluid, the white matter and the grey matter—are of different densities and accelerate and decelerate at different rates, so delicate structures connecting the layers stretch and shear and bruise.
And milliseconds after the explosion, a blast wave sweeps into the vehicle and bounces around, hitting the soldiers’ bodies again and again. These waves penetrate chests, constricting blood vessels, disrupting blood flow in the brain. They shift the bony plates of the skull, putting pressure on the brain. In response to these assaults, the brains swell, damaging more delicate structures.
Much of this damage takes place at the microscopic level, to axons, tiny projections on brain cells that transmit information. Just as it can take days for a deep bruise to make it to the skin’s surface, weeks and months can elapse between injury to the brain and when a soldier begins to notice things are awry.
That’s time enough for a new mission, to come within another blast’s radius, time for other injuries, for damage to be piled on damage.
Seeing Bedard nursing his neck, his comrades let him drive reconnaissance for the remainder of his tour. When he returned to Canada in August, he had 45 days of leave, and spent them in physical and psychological pain.
Shortly after returning to duty he was diagnosed with traumatic brain injury (TBI). The damage was not visible on a brain scan, but his symptoms were unmistakable. “The neurologist said ‘in four years this is either going to go away, or it’s still going to be there.’ That was the essence. They didn’t give me any treatment.”
The damage done to soldiers’ brains is not only hard to diagnose, it can be impossible to treat. Medical practices so far have not been completely up to the task, but scientists are working hard to get there.
In 2007, Bedard was also diagnosed with, and began treatment for, post-traumatic stress disorder (PTSD). He was medically released in 2010. He’s been in pain ever since.
“My whole head hurts. All the time. Like I’ve just been hit in the head with a frying pan.”
While diagnosis and treatment of other diseases and health conditions entered the space age, physical and psychological injuries to the brain have lagged behind. “In psychiatry, we’re still in the stone ages while the whole rest of medicine has moved forward,” said Colonel Rakesh Jetly, chief psychiatrist and mental health advisor to the Canadian Armed Forces surgeon general.
There is as yet no simple diagnostic test for either TBI or PTSD. There are no cures. Cognitive rehabilitation is the basis of treatments for TBI, aimed at slowly rebuilding attention, memory, social and emotional skills. The cornerstone of evidence-based psychotherapies for military PTSD is recall of traumatic memories, a process so psychologically painful that up to a third of patients drop out. Drugs are used to treat symptoms of both injuries. “And there are side effects…people stop taking them,” said Jetly.
Traumatic brain injury and PTSD have been around as long as armies, but there has been no objective way to diagnose them, like the blood test for diabetes diagnosis. It’s common for doctors to prescribe drugs designed to treat other conditions—antidepressants, anti-psychotics, anti-anxiety drugs, anti-seizure drugs and sedatives—for treatment of PTSD. A century from now, people are likely to look at how we treat brain injury today with the same horrified fascination we have for the leeches and bleeding of centuries past.
Medics, doctors and psychiatrists have had to rely upon soldiers’ self-reports of symptoms for diagnosis. And not being able to see exactly what was injured or how, they often resort to trial-and-error to see which evidence-based treatment, or combination of treatments, works in each case. Although most TBI and PTSD patients recover, a significant minority do not and live with chronic symptoms.
But that is changing. Recent developments in computing power and neuroimaging have put us at a new frontier in the study of the brain.
Helping veterans was one aim of U.S. President Barack Obama’s BRAIN Initiative (Brain Research Through Advanced Innovative Neurotechnologies) launched in 2013, and backed by at least $1 billion funding. It has grown into an international effort to plumb—and solve—mysteries of the brain.
The brain has nearly 100 billion nerve cells and 100 trillion connections, making it “one of the greatest mysteries in science and one of the greatest challenges in medicine,” says the BRAIN Initiative website. Five U.S. federal agencies and half a dozen foundations are funding research at dozens of universities and clinics as well as a whack of private industries. The armed forces in Britain, Australia, Canada, the U.S. and other countries, as well as philanthropists and veterans’ advocates, are also investing in neuroscience research.
Brain injury is a signature wound of modern war, the result of bullets and blast. Many more injuries come from rollovers and falls. And millions of military personnel and veterans suffer from a myriad of psychological injuries rooted in the rigours of their service—depression, addiction and anxiety at the top of the list. For soldiers with a brain condition, breakthroughs can’t come too soon or too fast.
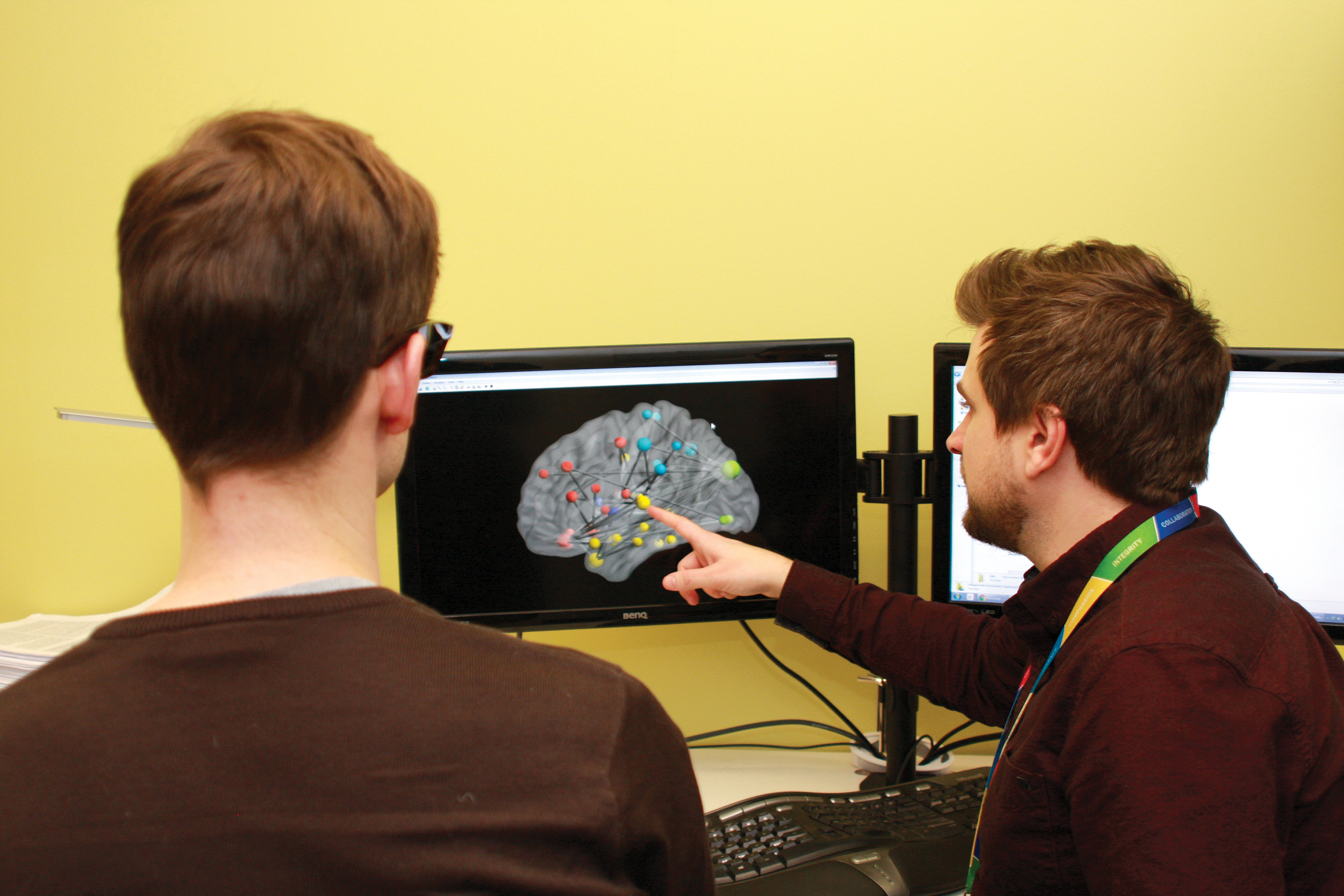
Progress is being made “at a staggering pace,” said Dr. Zul Merali, president of The Royal’s Institute of Mental Health Research in Ottawa. Research has already shown it’s not just that particular regions of the brain are damaged, but the way they communicate has been disrupted. “It’s actually the wiring within the brain that is not working well.
“Once we thought when brain tissue gets damaged, it’s gone permanently…never to be replaced,” said Merali. “Now we know new cells are being born every day, that circuits can reform, and the brain can find alternate pathways.”
The leader in military research is the United States, which has a quarter million serving military with TBI, where it’s estimated seven per cent of the nearly 22 million veterans have both PTSD and TBI, and 22 veterans die by suicide daily.
In Canada, about five per cent of serving military have PTSD, according to a 2013 Statistics Canada study. About five per cent of those who served in Afghanistan between 2009 and 2012 reported mild concussions—they were dazed or “saw stars”—and one in five developed post-concussive symptoms. But because concussions are vastly under-reported, nobody knows exactly how many of Canada’s 95,000 regular and reserve members have had concussions, let alone how many of the 600,000 veterans of all ages and conflicts.
There is no objective means to diagnose mild TBI (concussion) in the field. Symptoms can develop some time after the injury, be dismissed or put down to other causes. Treatment is more successful the earlier it starts. Risk goes up with combat exposure. After one TBI, risk of a second increases.
Not having a diagnosis at the time of injury (or having the record disappear in the fog of war or red tape) makes it harder to connect long-term symptoms to military service, raising the hurdle for qualifying for veterans’ benefits.
Scott Casey, who lives near Kamloops, B.C., developed PTSD after a tour in Croatia and Bosnia in the early 1990s. “I got out in 1994 and wasn’t officially diagnosed with PTSD until 2008. For that many years, I was a bloody mess.” Before he left the Forces, he was told he was suffering from anxiety. “That was probably a misdiagnosis.”
After he was finally diagnosed, PTSD treatment was painful and not effective. “I had to recount a lot of the horrible things that went on overseas. Reliving that stuff all over again was very difficult.”
Prescribed medication did not work. “I took to self-medicating, drowning my sorrows in alcohol.” He has strong opinions about drug therapy.
“Veterans are guinea pigs,” said Casey. “I think it’s safe to say if a soldier is prescribed a drug cocktail of 24 different meds every day, it’s probably not good for him.”
Bedard said, “They trialled me on 12 different ones and I had a nightmare experience.” He punched holes in walls, woke up “in pure rage.”
“The process took about three or four years. ‘Take some pills and go home. They didn’t work? We’ll try some different pills.’ The warnings all say they may cause suicidal thoughts.” Research shows one in two veterans with PTSD think about suicide and one in five attempt it.
He noticed flare-ups coincided with prescriptions meant to increase serotonin.
“Using drugs that aren’t designed for TBI, it’s playing with fire. They’re messing around with people’s brain chemistry.”
U.S. psychiatrist Dr. Peter Breggin agrees. “There is a strong probability that the increasing suicide rates among active-duty soldiers are in part caused or exacerbated by the widespread prescription of antidepressant medication,” he testified before the U.S. Congress veterans affairs committee. Breggin describes the “therapeutic effect” is to “chemically lobotomize” patients, an effect accepted by patients because apathy, indifference and loss of sexual function is an improvement over psychological pain.
“There isn’t a specific medication designed just for PTSD, so we’re borrowing from other areas,” said Jetly.
Confounding treatment is the fact PTSD and TBI have many symptoms in common—but the symptoms arise from different injuries, so need different treatments.
New technologies like PET (positron emission tomography), MEG (magnetoencephalography), fMRI (functional magnetic resonance imaging) and SPECT (single photon emission computed tomography) scans will allow amassing of information to tell which therapy works best for which injuries, said Jetly, the first to hold the Chair in Military Mental Health at the Canadian Military and Veterans Mental Health Centre of Excellence in Ottawa. Tailor-made treatment for each individual can then be checked by neuroimaging technology to see if it’s working.
It’s hoped neuroimaging will reveal exactly what structures have been injured and how they can best be healed, repaired, retrained or their functions augmented.
Research is establishing how brains affected by TBI and PTSD work differently from healthy brains, and from each other (The Tell-tale Brain, May/June).
Studies at Sick Children’s Hospital (SickKids) in Toronto sponsored by the Canadian Armed Forces and Defence Research and Development Canada compare brain activity of four groups: healthy civilians, combat soldiers who developed PTSD after trauma and trauma-exposed soldiers who didn’t develop PTSD, and civilians with mild traumatic brain injury (mTBI).
Early results reveal some regions of brains affected by PTSD are overactive, and that veterans with PTSD see threats everywhere. While all soldiers reacted to combat-related stimuli, the PTSD group had a markedly greater response. “Their brains are in a hyper-aroused state,” said Dr. Margot Taylor, director of functional neuroimaging in the Department of Diagnostic Imaging at SickKids.
Another study showed PTSD sufferers reacted more strongly to angry faces. Communication among regions of the brain controlling fear and emotion were overactive, while the part that inhibits fear was underactive, said Dr. Ben Dunkley, clinical associate in diagnostic imaging at SickKids.
“One of the problems in diagnosis is that mTBI or PTSD or psychological trauma don’t leave structural or anatomical scars that you can see on an MRI.” However, they do change the way regions of the brain communicate. MEG shows some brain waves of those with combat-related PTSD are hyper synchronized and “talking to each other constantly,” said Dunkley. “Even at rest, they’re not silent.”
Why is not yet known—so neither is what to do about it. Yet.
Captain Adrian Rizzuto volunteered for the study to help find answers for comrades and friends.
After he returned from a tour to Afghanistan in 2008-09, he was unable to sleep more than four hours at a stretch. “I was barely functioning.” Worried it might be a harbinger of PTSD, he sought help. It turned out to be a transient sleep disorder relatively easily treated. But it reinforced the need for faster diagnosis. “It’s important we have a diagnostic test that says ‘this person is clearly suffering from PTSD, and here’s the brain scan to prove it.’ Right from the beginning, when they realize something is wrong and are figuring out how to treat it, right up to the end when they need help from Veterans Affairs Canada, a test will help.”
Mark, who prefers not to be identified, volunteered to help research tease apart PTSD from TBI symptoms. “I know the symptomology has a lot of overlap. A reliable diagnosis is important because people whose symptoms are from different causes will be able to have the proper care.” For instance, both TBI and PTSD cause sleep disturbances, but medication for PTSD sleep deprivation might over sedate someone with TBI.
“We know in 80 per cent of people with mTBI, problems with memory and attention spontaneously disappear in less than three months, but 15-20 per cent will have lingering symptoms that are chronic and really affect people’s quality of life. These head injuries are thought to damage the axons that send information between regions of the brain,” said Dunkley. “These injuries are microscopic and diffuse and can’t be picked up by MRI, but affect how neurons fire and talk to one another.” And that can be tracked by MEG.
Mark is lying on a bed at SickKids, his head inside something resembling an oversized, old-fashioned hair dryer lined with sensors called magnetometers that catch the tiniest changes in the brain’s magnetic field. The room has foot-thick walls. “The brain’s magnetic field is so minute, it would be completely flooded by environmental noise,” explains Dunkley. “So we have to keep them (Mark and MEG) in a large magnetic shield.”
In the room outside, computer-generated images of Mark’s brainwaves play across a monitor, changing as his brain works when he’s given different tasks—matching colours or shapes or images. The machine is so sensitive that tiny blips appear in the regular oscillations whenever Mark blinks. Afterwards, he goes through similar mentally challenging tasks in an fMRI, which captures images of the brain as it works. “We meld the data from the two machines,” said Dunkley, to find out what is going on in the brain, and where it’s happening.
Mark suffered a concussion while cycling in Toronto when a passenger opened a door in front of him. He tried to carry on with his day, but was eventually persuaded to get medical help. “I actually didn’t believe the doc when he told me I had a concussion,” even though he had noticed everything on his right side looked brighter. “I didn’t get the full effect until the day after.” He had a whopper headache, and “really weird visual disturbances. Everything was jittery.” He found himself emotional, irritable and impulsive. He had suffered diffuse axonal injury. “The way the neuro optometrist put it, it’s like the cables that run from my eyes to the occipital lobe (in the brain) are frayed.”
Recovery has been a long process. “It’s really not up to you how fast you recover. I always thought my recovery was a week away, then two weeks away. And now it’s two years. You can have a good day, and the next day be down for two weeks.” He wears a mask and ear plugs, and still doesn’t get enough restful sleep. He has a headache that varies in intensity, but never goes away. He’s really sensitive to light. He can’t drive on bad days. He’s still not able to go back to his job.
Aside from helping with diagnosis, brain scans may eventually be used to determine when someone is able to return to work, and when they need more time to heal, said Dunkley.
Perhaps one day brain scans can be used not only to detect atypical brainwaves, but to help bring them back to normal by targeting areas for deep brain stimulation. Perhaps they will help identify subtypes of PTSD and TBI. “We’re really only scratching the surface of what we can do with these technologies.”
It’s early days yet.
A gene has been identified that appears to predict who will develop severe PTSD symptoms. It is linked to a thinner cortex in brain regions that help humans cope with stress and trauma and control strong emotions. “In future, it may be possible to use a genetic blood test to identify military personnel at risk for developing PTSD” in war zones, Naomi Smith Sadeh, a psychiatry professor and psychologist at the National Center for PTSD for Veterans Affairs in Boston, said in media interviews. The research has implications for prevention of PTSD, targeted intensive treatment and suicide prevention for those with the gene.
Research is showing more clearly what is damaged. University of Washington scientists found tiny leaks in the blood-brain barrier develop in the cerebellum of mice exposed to blasts, leading to inflammation of microglia, primary immune cells of the central nervous system. This damage may lead to later development of neurodegenerative disorders like encephalopathy and Alzheimer’s disease, connections being studied in Canada, Australia and the U.S.
Diagnostic tests for both PTSD and TBI are expected within three years.
Metabolomics—using a computer to assay minute chemical differences in blood samples—identified 95 per cent of concussions in a study of male hockey players, Dr. Douglas Fraser of the Children’s Health Research Institute in London, Ont., reported at the Canadian Institute of Military and Veteran Health Research Forum in 2015. Jing Zhang, of Royal Military College in Kingston, also reported that RNA (ribonucleic acid, which translates the genetic code for use by cells) might serve as a biomarker for TBI, based on studies showing micro RNA in rats’ hair follicles was silenced or degraded by blasts.
“I think it’s safe to say if a soldier
is prescribed a drug cocktail of
24 different meds every day, it’s
probably not good for him.”
PET/CT scans show pituitary glands of veterans with PTSD are working extra hard, report researchers at the St. Louis University School of Medicine studying the HPA axis—the interconnection of the pituitary gland and the hypothalamus in the brain and the adrenal glands, which sit above each kidney. The axis regulates stress response, mood and energy expenditure, and is suspected of playing an important role in PTSD. Damage to any of the three affects the others.
“This raises the possibility that some PTSD cases are actually hypopituitarism” and can be treated with hormone therapy, Dr. Thomas Malone, of the university’s neuro-surgery department, reported to the Radiological Society of North America in 2014. A study funded by the U.S. Department of Veterans Affairs found 44 per cent of veterans with blast concussions also had low levels of pituitary hormones. “If the possibility of hormone deficiencies in our veterans is not considered, appropriate treatment may not occur,” said lead researcher Charles Wilkinson, of the Veterans Affairs Puget Sound Health Care System in Seattle, Washington.
Developments in treatments may take longer.
Deep brain stimulation has dramatically reduced PTSD symptoms in the first veteran to undergo the procedure, doctors at the VA Greater Los Angeles Healthcare system reported in 2015. A pacemaker-like device was implanted in a veteran’s brain to stimulate his amygdala, which is involved in the fear response. After 10 months of treatment, the 48-year-old Gulf War veteran, who had not responded to years of other treatments, reported dramatic improvements in the ability to sleep, mood and emotional control and number of nightmares. But it will be years before the treatment enters the mainstream.
A few dozen volunteers have had small electrode arrays implanted in regions of the brain involved in recall, spatial memory and navigation to improve memory through electrical stimulation of the brain. Early results of the Defense Advanced Research Projects Agency (DARPA) project are encouraging, and researchers are now trying to determine whether stimulation is best used while memories are being stored or retrieved. “These early experiments are clarifying (such) issues and suggest there is great potential to help people with certain kinds of memory deficits,” program manager Justin Sanchez reported at the 2015 Wait, What? A Future Technology Forum.
DARPA hopes eventually to capitalize on brain plasticity, the brain’s ability to reorganize neural pathways to compensate for injury, to develop implants that can address neuro-psychological illness.
But eventually is not fast enough for the soldiers and veterans living with TBI and PTSD. Alarmed by the sheer numbers needing treatment, and the limited number of U.S. Veterans Administration facilities, the Intrepid Fallen Heroes Fund financed the National Intrepid Center of Excellence (NICoE), which opened in 2010 near the Walter Reed National Military Medical Center in Washington, D.C. And it is building nine Intrepid Spirit Centers, five of which have already been completed, to diagnose and treat serving military personnel and veterans with TBI, PTSD and other operational stress injuries. Centres, each located near a base, will cost $11 million to build and equip. While NICoE is devoted to research, Intrepid Spirit Centers focus on diagnosis and treatment.
Medics, doctors and psychiatrists have had
to rely upon soldiers’
self-reports of symptoms for diagnosis.
In Canada, veterans advocates are pushing for the two veterans’ national health care centres of excellence promised by the federal government to be devoted to mental health care.
“There are hospitals already on the cutting edge of physical injuries,” said Bedard, who is on a VAC veterans advisory committee. But there aren’t enough dedicated facilities addressing veterans’ mental health. Now veterans with PTSD are treated mostly by civilians who may have no concept of military culture, or in facilities that mostly deal with rehabilitation of civilians with addictions. Veterans have long advocated for treatments, programs and specialists sensitive to military culture, ideally in dedicated facilities. The two new centres could fill the bill, said Bedard. And they could be a focus for research on military mental health care, which is now spread out among a number of universities, hospitals, institutions and private industries.
“We could keep two mental health centres running full-time forever,” he said. “We currently have 1,300 members in Joint Personnel Support Units, and if half have PTSD, that’s about 750. Then you have to catch up for people who’ve been released. And then you could serve corrections officers, RCMP and first responders.”
Bedard hopes the full panoply of positive results of neuroscience research will play out, but diagnostic tests would immediately improve the lives of thousands of veterans.
Not only would it get them into treatment faster, but it would help overcome stigma.
“At the end of the day, we can’t cure anything,” said Bedard. “We can’t make symptoms disappear. The very least we can do is reach out to show these invisible wounds. Hand them proof they can take out onto the street or into the local [Royal Canadian] Legion branch, to the people who say ‘Well, you don’t look like there’s anything wrong with you.’ At least you have something in hand to say ‘Yeah, there is. Absolutely.’”
How far can it go?
Military brain research has a dual personality and purpose: to address health issues for serving members and veterans—and coincidentally, civilians—and add to the military’s technology arsenal.
Military research is leaping ahead in the quest to make stronger, faster, smarter troops with ultra human stamina—and the brain is a research destination.
Tens of thousands around the world now have brain implants that deliver tiny electric impulses to stimulate different areas of the brain, just as a pacemaker stimulates the heart. Such stimulation can be used to treat depression and post-traumatic stress disorder, stave off epileptic seizures, and allow people with Parkinson’s better control over their movements.
Research is also being conducted into use of implants on the battlefield, such as coupling implants to wireless communication so one day troops on the battlefield might be able to communicate by thought alone.
Transcranial magnetic stimulation, in which a tiny electric current is passed into the brain by a magnetic field, outperformed coffee in improving air force volunteers’ attention spans, alertness and accuracy in tests at the Wright-Anderson Air Force Base in Ohio. A helmet filled with electromagnetic coils has already been approved by the U.S. Food and Drug Administration for use in treating depression, and researchers hope to develop more user-friendly units that resemble music earbuds or can be used like a phone app. “We’re beyond proof-of-concept phase,” biomedical engineer R. Andy McKinley said in a Boston Globe story. “We’re working on something that would be easy to apply and that you could potentially [use in the] field.”
DARPA’s Neural Engineering Systems Design Program is working on a brain/computer interface to convert electrochemical language of neurons into computer language. Capable of connecting with a million neurons, it’s only the size of the button on a man’s suit jacket. On one hand, it could improve thought-controlled prosthetics for amputees and allow doctors to monitor patients between visits, and on the other, allow troops to control equipment or help soldiers better detect danger on the battlefield. Brain implants could link pilots to computers to speed up reaction times when dealing with overwhelming amounts of data.
But while there might be wide public support for use of such technology to relieve symptoms of Alzheimer’s disease or dementia, enhancing brains of healthy people might cause some public concern. It’s one thing to stimulate brains of navy technicians so they can quickly synthesize information coming at them simultaneously from computer screens and telephones, but what about using such technology so an elementary student can master the times tables?
Neurotechnology “raises a lot of questions we’ve just not had to face before,” said Jonathan Moreno, a bioethicist at the University of Pennsylvania and author of Mind Wars: Brain Science and the Military in the 21st Century. “When existential survival is the issue, then people are generally more favourable to enhancement, because the stakes are so high, whereas with small children, your tolerance may be less.”
The United States is a research leader, partly because of President Barack Obama’s billion-dollar BRAIN Initiative, partly because of the duty to protect the health and safety of its 1.5 million citizens in uniform and nearly 22 million veterans. The U.S. also wants to avoid technological surprises that raise security threats, such as the 1957 launch of Russia’s Sputnik which sparked the space race.
The U.S. Department of Defense and DARPA are also spending billions on brain research to enhance performance of personnel and decrease effectiveness of foes. They are exploring technology and drugs that would allow soldiers to go a week without sleep, to suppress fear, extend alertness and ignore pain. And exploring neuroweapons, such as drugs that could be sprayed on the enemy during battle, causing them lose their fighting spirit (or consciousness) and lay down their arms. Where will it all lead…and where will it stop?
“I think you could get an international convention that would prohibit amputating limbs so you could put on better ones,” said Moreno. But an exoskeleton like the one that can help Trevor Greene, the Canadian soldier who suffered severe brain injury in an axe attack in Afghanistan to walk, “that’s a different party.” (“A Mighty Big Bionic Step,” January/February 2014).
Expense will be carefully weighed against usefulness. “We’re so depleted in basic stuff like trucks and tanks [that] they’re not installing biosensors in helmets. The people buying this stuff have to be convinced it solves a problem better than something else. Why use a laser to blind someone, when you can just shoot them?”
And there’s fear of increasing dependence on technology. The last thing any commander wants is for pilots or infantry to become over reliant on technology that can be interrupted or fail on the battlefield.
“When I close my eyes and go to sleep at night I’m not mostly worried about this stuff,” said Moreno. “Some people think that anything I wrote about in Mind Wars is going to be done. Actually, very little of it will be done outside the laboratory.”
Advertisement