In any given year, about a third of Canadian Forces personnel are laid up some time or another by strains, sprains, broken bones and similar injuries. These injuries account for 41 per cent of chronic health conditions, 53 per cent of medical releases and about half of Veterans Affairs Canada benefit claims.
On any given day, 35 to 45 per cent of those on sick parade are suffering from MSK—musculoskeletal injuries. Sprained ankles, strained knees and sore backs do not garner the attention of mental health issues or battle wounds, but such injuries are a serious issue. “MSK injuries are one of our top medical problems,” says Dr. Maureen Carew, public health physician with CF Directorate of Force Health Protection. In 2008, 36 per cent of Forces members reported an injury serious enough to limit normal physical activities.
“It affects our operational readiness,” adds Lieutenant-Colonel Peter Rowe, CF national practice leader for physiotherapy. MSK injuries accounted for just under a third of those unable to deploy in the previous two years. Reducing injury would increase the pool of deployable troops and reduce non-battle injuries while deployed.
Research on personnel deployed to Bosnia a decade ago revealed MSK injuries are not always resolved before leaving Canada. “Probably about 30 per cent of the people deploying (who had been) seeing a physiotherapist were deploying with a chronic condition,” says Rowe. The danger is that low-level injuries become worse in theatre, where troops wear heavy body armour and are carrying around equipment for long periods of time. Even clerical staff are not immune—longer work days with fewer rest days increase risk of repetitive strain injury. Although Canadian data is lacking, MSK and connective tissue injury was the most common reason for medical evacuation of United States soldiers in Iraq and Afghanistan between 2004 and 2007.
MSK costs the CF at least $21 million annually in lost wages alone, but the price tag is probably much higher, says Carew, since those statistics only reflect those off work for three days or more, and do not include treatment and rehabilitation costs—prescriptions, surgery, physiotherapy and chiropractic treatments.
But it needn’t be so. “Injuries are not accidents. They are preventable,” says Carew, who presented a report on the CF’s burden of injuries to the Military and Veterans Health Research Forum in Kingston, Ont., in November. Rowe spoke on the impact of MSK at the forum.
Ironically, Rowe reported, most MSK injuries occur on the playing field, not the battlefield. Physical fitness is a big part of military culture; it keeps personnel in shape for operations, promotes esprit de corps and unit cohesiveness. In keeping with this, The Royal Canadian Legion sponsors the CF Sports Championships and gives an award to the most sportsmanlike person in each category.
All personnel need to pass an annual physical fitness test. But in a culture that prizes strength of body and character, many push themselves to do much better, increasing the risk of injury from overtraining, says Rowe. Sports and physical training accounted for 52 per cent of acute injuries in 2004—and running is a major culprit.
Military health research has resulted in changes to running regimes and footwear, says Rowe. It shows when stress fractures are likely to occur in a progressive running program, and when lowering intensity and frequency allows bones to recover, preventing fractures. Orthotics that cushion and support the foot, redistributing pressure, also help prevent injuries. Armed forces in many countries are changing how they go about group runs; dividing a unit into three groups allows the highly fit and practised to work harder while reducing the risk for the less accomplished who no longer feel pressured to perform above their skill level.
Research is also helping determine best injury treatments, he says. Injured personnel used to first see a doctor for diagnosis and referral for physiotherapy. Now physiotherapists and chiropractors are located at many military health centres, allowing for quicker and more appropriate treatment. Therapists in uniform have an edge over civilian practitioners, says Rowe. “When I say ‘you’re doing rucksack marches and do this and this’ (to prevent injury), patients know I’ve done rucksack marches” and take the guidance to heart.
In 2009, more than 20,000 of the CF’s 68,000 regular force personnel were assessed by physiotherapy, resulting in 100,000 treatment sessions. Research shows in-garrison treatment is more efficient. Patients treated off base average 11 treatments, compared to five for similar injuries treated on base.
But there’s work to be done to cut injury rates. “People accept injuries as normal,” says Carew. Although 61 per cent of respondents to the Health and Lifestyle Information Survey said their most serious injury could not have been prevented, the Australian armed forces found small changes produced big results. Modifying training regimens cut injury rates by 30 per cent, use of braces on sports courts and mouth guards during hockey games halved injuries, as did ankle braces for parachutists.
The CF is testing an injury surveillance system at Valcartier, Que., that will allow health services to spot injury trends, suggest changes to injuries, and measure if the changes have been successful. If the pilot project pans out, the program could be rolled out to bases across the country.
Future research will include analysis of complete economic and medical costs of non-battle injuries, and programs to communicate the data and educate troops and the chain of command about prevention.
“When it comes to non-battle related injury, we haven’t been doing a good job of communicating the information,” says Carew. “Injuries are preventable.”
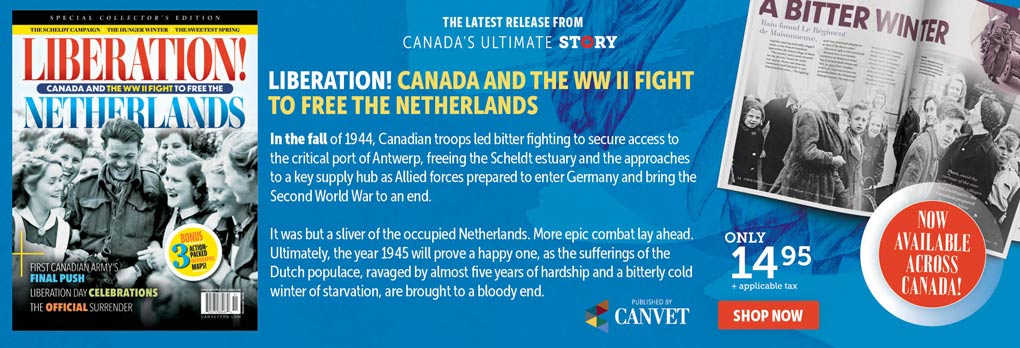
Advertisement