![[ILLUSTRATION: DAVID JUNKIN]](https://legionmagazine.com/wp-content/uploads/2013/03/PTSD1.jpg)
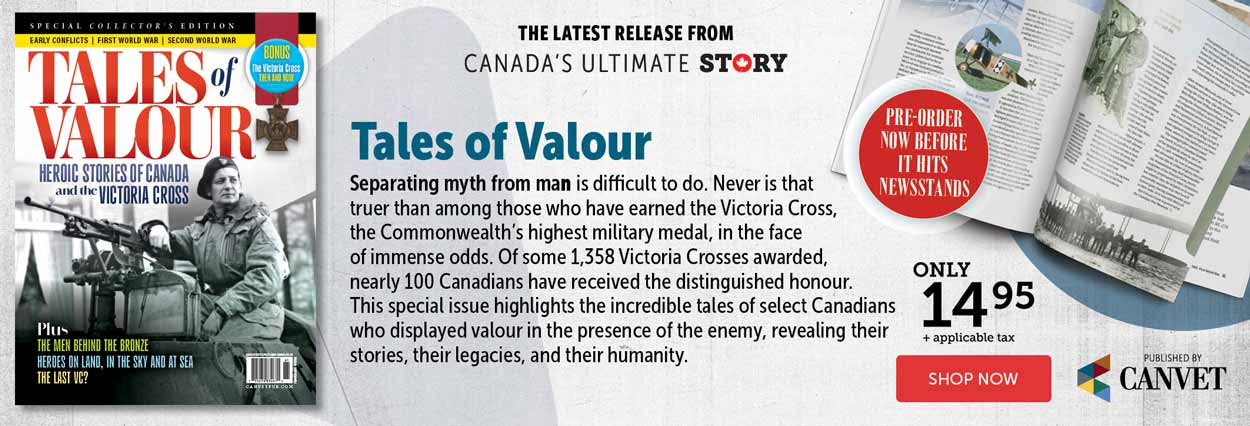
Exclusive Audio Edition:
Andrew is hiding inside his jacket. He’s hunched over, clutching his gut, clearly in distress. He keeps his head down, his face obscured by a ball cap with an overly large bill. An early arrival, he’s snagged the chair in the corner across from the door, the safest chair in the room. It’s a small room, and at the moment it’s hot with anger.
Nine men—soldiers, sailors, airmen, veterans—have come to this meeting in Halifax to talk about living with PTSD—post-traumatic stress disorder. They’ve all got it, and they mean to talk about it, but can’t muster the right emotions at this moment. A few of the angriest have hijacked the conversation and can’t be moved from their litany of grievances against The System, whichever one they’re fighting or have fought. In a room full of strangers, it’s a useful shield to ward off the reopening of old wounds.
Only a few of them have met before, their paths crossing sometime during their military careers or in therapy. They all know Dr. John Whelan, the psychologist and PTSD researcher who has provided a room for the meeting. Whelan was a naval electronics technician in the 1970s and ’80s before he trained for a career in psychology. Former Atlantic clinical director of addiction services for the Canadian Forces, he went into private practice in 2004, specializing in PTSD treatment for military personnel and veterans. He has street cred with this group; it’s why they’ve volunteered to share their stories with a journalist, rounding out a series of interviews with other veterans coast to coast.
Only three of the men agree to be named. There’s retired Chief Warrant Officer Jean-Guy Trudel, whose gentle voice and calm demeanour are at odds with his tough-guy appearance. Sitting next to him is retired Master Warrant Officer Steve Dornan, a former airborne electronic sensor operator and intelligence field analyst. Dornan is a calming counterpoint to former paratrooper Bill Maguire, whose anger bristles like quills on a porcupine. The veterans in this room range in age from their thirties to mid-sixties and represent all three branches of the service. Several have, in fact, served in all three. Maguire is the oldest, his career spanning 37 years and two services. He’s had tours to Cyprus, the Middle East and Somalia and he’s had to do his share of shitty duty on home soil, too. He has little patience for political correctness and calls things as he sees them, hurt feelings be damned. The anonymous speakers include a submariner who served in HMCS Chicoutimi in 2004 when the sub caught fire, a former intelligence officer, an Army veteran currently in a fight for benefits and a couple of veterans who don’t want their trades or services revealed because that will give away their identities. Some have never told friends and family about their experiences.
Anger envelops the group, voices rise and F-words multiply, but Andrew still hasn’t said a word. Then someone says he’s dying for a smoke, a Navy vet says he’s gotta hit the head, and they agree to take a break. The emotional tension rushes out of the room with them, like air in a deflating balloon. Andrew is first to shoot out the door, and everyone thinks that’s the last they’ll see of him. But he’s the first back in, the scared-deer look gone from his eyes, replaced with something approaching determination. Or maybe desperation. He’s the first to speak, words rushing out like steam escaping the safety valve of a vessel about to blow.
“I thought it was normal to be angry all the time, going through life basically holding it in to the point after so long where I would explode,” says Andrew. “I would have given my life for my country,” he adds, “and I would rather have done that than to have experienced this.”
Andrew has lived with PTSD for half of his life, starting with his first tour, at 19, to Bosnia in 1993. He and a buddy were injured by what they then called a booby trap and what we know today as an improvised explosive device (IED). The other soldier had serious shrapnel wounds and was airlifted to hospital, then back to Canada. Andrew was around the corner of a building, protected from shrapnel but not the blast wave, which knocked him unconscious. He awoke with a terrible concussion headache, ringing in his ears and blurry vision. They wanted to send Andrew home, too. “But being 19, I fought tooth and nail,” he said. He was a small-town boy with big dreams, proud of his uniform. After a few days his vision cleared and the headache disappeared. Then the nightmares started. Little was known then about the damage a blast wave can do to the human brain, or that it increases risk of PTSD. The nightmares accumulated, got progressively worse. Andrew was serving in the Medak Pocket during the bloodiest period of the civil war in Bosnia. Though armed and trained, the Canadians on that United Nations mission couldn’t intervene in a massacre they knew was going on. Serbian and Croatian forces agreed to a ceasefire, and French and Canadian troops were assigned to supervise withdrawal of the opposing forces. Although gunfire and explosions could be heard in nearby villages, local Croat forces refused Canadians access to the area and opened fire on their UN vehicles.
That mission marked the beginning of Andrew’s slow downward spiral as the shining career he dreamed of began to slip away. The other men in the group make supportive sounds as he describes how his life fell apart as his symptoms worsened, affecting his performance during the remainder of his six overseas tours of duty. He struggles to hold in tears when he talks of the days when nobody believed he had PTSD, when they thought he was just a chronic bad actor with a drinking problem. He talks of feeling alone and betrayed. “The biggest slap in the face for me was all these people I worked with, who knew me for years, knew I was a hard worker. All of a sudden the wheels fall off and not one person stepped up and said, ‘Hey, what’s going on?’ I would have had anybody’s back at any time.” It hurt to think that nobody had his.
He talks about the fight for diagnosis, about the civilian psychiatrist who thought he was lying about his experiences. “How could he know? He went to head-shrinking school. His 19-years-old was going to university and chasing girls.” The battles Andrew fought overseas were bad, PTSD was bad, but the battle to get help nearly did him in. He describes the night he struggled with the decision to kill himself. After a short silence, someone asks how many others in the room know someone who’s committed suicide. They all put up their hands. How many have thought of suicide themselves? Most hands go up again.
Andrew has blazed the way, and one by one, the others share their stories. They talk of isolation, grief, shame. Feeling betrayed. They describe how symptoms tore apart their lives, damaging marriages, fouling relationships with children, ending careers. They speak of symptoms that walked them through hell: losing the ability to sleep, about nightmares that feel frighteningly real, quick-trigger tempers. And about treatments that are a torment, but have led most to a calmer place. By the end of the meeting, everyone is physically and emotionally exhausted. They may have begun as strangers, but in sharing their stories they’ve come to recognize they’re fellow travellers. They’ve all crossed a border into a land foreign from everyday life, and have had trouble finding the way home.
Across this land, many people with military backgrounds have crossed that border, their lives shaped as much by their interior landscape as by where they live. A veteran in Calgary said it doesn’t matter where he is or what he’s doing, he spends part of every day back in Afghanistan. It’s as if they’re PTSD prisoners of war, denied the luxury of ever coming home completely. It’s not just that they’ve been changed by the experience; some describe it as losing a piece of themselves. The public is used to seeing military amputees with prosthetic legs and arms—but who can fashion a prosthetic for a missing piece of self?
The same values that spur soldiers to help the wounded during a firefight drives veterans with PTSD to share their stories. They want to encourage others to get help, to understand they’re not alone, to see it’s possible for things to get better. They want more and better services for military personnel, veterans and their families. They want conditions to change so PTSD can be prevented in more cases and they want treatment and support to improve. “I’m a very private person,” said Andrew, “but I don’t want nobody else to have to go through this. It’s killing me right now just thinking about it. [My story] might help someone else.”
![[ILLUSTRATION: DAVID JUNKIN]](https://legionmagazine.com/wp-content/uploads/2013/03/PTSD2.jpg)
Over the next five years or so, approximately 30,000 personnel will leave the Canadian Forces. It’s expected that about a third will have mental health issues, such as depression, anxiety, addictions and sleep disorders. Of those, nearly 3,000 will have severe PTSD. No one knows how many veterans of previous conflicts have PTSD and never sought treatment. When the next Afghanistan, the next Bosnia or Cyprus or Rwanda comes around, there will be a new generation of PTSD casualties, and veterans who’ve shared their stories want to make sure help continues to be available.
Descriptions of PTSD appear in the earliest written accounts of warfare, and it has had many names throughout the centuries: the thousand-yard stare, soldier’s heart, shell shock, battle fatigue, combat stress. Although tens of thousands from the First World War and the Second World War suffered PTSD, shortly after those conflicts ended attention of politicians, the military and the public shifted to other priorities. It didn’t take long for research into what causes PTSD and how best to treat it to stop. Modern veterans worry that current interest in PTSD will languish once their battles fade from memory. They worry about funding cuts—that as money dries up, the search for more and better treatments will evaporate.
There is reason to worry. The system is strained. A 2011 CF Health Services report titled Cumulative Incidence of PTSD and other Mental Disorders warned of chronic staff shortages and of vulnerable funding jeopardizing mental health services. There have been news reports about threatened closures, even of the unit that houses suicide-prevention specialists, and of possible staff cuts to the section that researches issues like PTSD, depression and suicide.
“The OSI (Operational Stress Injury) burden remains at peak intensity and will continue at this level for several years yet,” said National Defence and Canadian Forces Ombudsman Pierre Daigle in Fortitude and Fatigue, his 2012 assessment of the CF’s mental health care system. Although new mental health policies and programs between 2002 and 2008 have reduced stigma and improved detection and treatment, the CF struggles to meet needs. There’s a chronic shortage of mental health professionals, Daigle reported. In 2005, $98 million was committed over five years to increase the number of mental health-care providers to 447 from 229. It hasn’t happened, not least because there is a national shortage of mental health workers, including psychiatrists. In September the CF counted 378 military and civilian mental health-care providers.
In September, Defence Minister Peter MacKay beefed up the CF’s mental health budget by $11.4 million, bringing it to approximately $50 million annually. The new funds are for recruiting more mental health-care professionals and cutting wait times. In a speech at the Military and Veterans Health Research Forum in Kingston, Ont., in November, he talked about the importance of partnerships between government departments, academic researchers and allies whose troops are experiencing the same problems. But the global economic situation has touched all these partners, too; budgets are being slashed everywhere. “It’s not just tanks and battleships that are cut—it’s medical research…health care and disability care,” said psychologist Bret Moore, co-author of Treating PTSD in Military Personnel. A veteran and former U.S. Army psychologist, he has seen what funding cuts can do to research.
“Our understanding of the condition is…imperfect,” stated a 2011 Library of Parliament report on military and veteran PTSD, “and there are no certainties, except for the distress of those affected.” For much of Canadian military history, PTSD sufferers have had to handle that distress pretty much on their own.
Second World War veteran Stewart MacDonald has soldiered on alone with PTSD for more than six decades. The Cape Bretoner was just 18 when he went to war. It’s what teenaged boys did, or yearned to do, in 1944. Patriotism and duty aside, it was a chance for them to prove something, to take part in something bigger than themselves, and an opportunity for adventure, a rarity in the life of a small-town kid from the Maritimes. MacDonald spent two years in Europe as the Canadian Army liberated Holland and pushed into Germany.
As for most combat soldiers, death was ever close. Machine-gun fire stitched through the backpack worn snugly against his spine, a soldier walking near him stepped on a landmine, a shell pulverized men in the next room of a sheltering house. He was given the job of searching through basements, to roust out enemy troops. He found none, but he did find bodies of mothers, their arms in futile protective embraces around their dead children. He saw more dead mothers and children along roadsides, in fields. He saw Germans, young men his own age, shot as they tried to surrender. All this before he turned 20.
MacDonald returned to Canada and peacetime, but the war never left him. “I had bad dreams for years and years and years,” he said. “The nightmares were horrible. Bombings. Shootings. I’d wake up and my sheets would be all wet. And I’d be fighting with myself. I was afraid to stay in boarding houses or hotels. It went on even after I was married. My wife, she had to put up with a lot.” A teetotaller all during the war, he climbed into the bottle when he got home. “I don’t want to talk about them days. They were my worst, worst, worst days ever.” He didn’t know where to go for help, so like thousands of others, he went to the beer parlours and Royal Canadian Legion halls to share his stories and ask buddies what they were doing about the nightmares. He was advised to put a bible under his pillow.
One veteran in Newfoundland said he’s willing to share his story because he wants someone to tell the truth about PTSD. But there appears to be no one truth, and the telling won’t be easy. PTSD can be caused by different kinds of trauma, but not everyone who experiences trauma goes on to develop it. It can take years for symptoms to appear. Two people who develop PTSD after the same event may have different symptoms. There is no one treatment, no one drug, no combination of drugs and treatment that works for everyone, so it can take a long time to find relatively effective therapy. Even after treatment, a minority of people have persistent symptoms that prevent them from living a normal life. There is no cure, and perhaps there can be no cure. “PTSD is not a disease,” said John Whelan. What inoculation protects a soldier from wounds, what salve erases bullet scars, what medicine restores missing limbs? As with other bodily wounds, PTSD leaves scars—but they are not visible.
Until relatively recently PTSD was often dismissed as weakness in moral character, even cowardice. That idea was finally scotched in 1980 when PTSD was added to the Diagnostic and Statistical Manual of Mental Disorders, its cause listed as a traumatic event followed by severe emotional reactions such as panic, terror grief or disgust. It took time for the military to accept PTSD as a wound, then build up services to treat it. Now the Canadian Forces recognizes four causes of Operational Stress Injuries, of which PTSD is the most severe. It’s not unusual to find people who’ve suffered more than one, or even all four.
Events that provoke terror, horror or hopelessness. Retired Master Warrant Officer Steve Dornan only hints at the horrors of his assignment in Bosnia, which involved locating mass graves of massacre victims. “It was very easy to tell,” he said, “because there’s human remains sticking out of the ground.” Retired Chief Warrant Officer Jean-Guy Trudel believes the slow accumulation of stress over his 37-year career—constant moves, ever-increasing responsibility, seeing too many disturbing sights on tour—ripened him for PTSD. On deployment in the late ‘90s he got word a friend had killed his wife with an axe, then hanged himself. “I just compartmentalized it, put it aside,” he said. “I didn’t heal right, in retrospect.” The first night he returned from a tour of duty he had a terrifying nightmare about killing his own wife. “I took all of my axes, put them in the trunk of my car, went to base and put them in a dumpster. That’s how scared I was and how vivid the nightmare was.” Shortly afterwards he went into the base woodshop and accidentally sliced the tips off two fingers in a planer. By then he was so emotionally numb he didn’t react normally even to that. In Bosnia, he saw a school with lines of bullet holes about 18 inches up the walls. “That’s where they were killing the kids, just the little guys.” In Haiti he saw children picking through storey-high piles of garbage, looking for things to sell to feed themselves. “That was the last straw.” He sought therapy in earnest, and retired sooner than planned.
Stress accumulated over time. Sergeant Ted Peacock hadn’t caught his breath after returning from Afghanistan in 2005, where his unit had been at the receiving end of regular attacks, when he was asked to go back. “I said ‘this is like six years now and I’ve just been going, and going and going, so when I come back I kind of want a break. And they were like, ‘yeah, everyone needs a break.’” On the next tour, the Albertan took over even heavier duties after the warrant officer was injured by an IED. When he got home, instead of the requested break, he was given a new assignment. “On Friday, I was told that I was going to be the operations warrant (officer) for a field squadron. On Monday I said I needed help, and “they said, ‘OK, here’s a couple of sleeping pills.’ So I came home and got drunk and just freaking broke down. I destroyed my garage. I went from one day having all this emotion in me and crying and yelling to just…nothing.”
Grief. “We all arrive with a certain amount (of resilience) in the bank, some more than others,” said Philip, a major from the Prairies who served a tour in Afghanistan a half dozen years ago. Part of his unit’s duty was to reclaim equipment, cleaning it up after an IED event, a shooting, a traffic accident. He remembers once entering a light armoured vehicle that had been hit by an IED. “There was a giant hole where the driver’s seat should be. I looked up and said, ‘Oh, yeah. Brains.’” One day he abruptly lost computer communications. Some years earlier, news of a fatality was leaked by e-mail back to Canada and became public knowledge before relatives could be informed. Since then, silenced computers had been a harbinger of death. His unit gathered, waiting for a name, and when it came it was not only someone they all knew, but a young corporal Philip liked and respected. Someone would have to reclaim his equipment. Looking at the stunned faces of his men, Philip said: “I’ll go.” The equipment had been put inside a yellow plastic bag, closed up in 41-degree heat. When Philip opened the bag, the stench of death enveloped him, burned into his brain—seared his soul. Grief emptied his resilience account. He is still in therapy.
Moral injury. It can be blatant, as for the peacekeepers in Bosnia who were prevented from intervening in a massacre. The crusty veteran Bill Maguire was profoundly shaken by the October Crisis, when Prime Minister Pierre Trudeau invoked the War Measures Act and called out the Army; troops faced the possibility of using arms against fellow citizens. Or it can be more subtle. “I’d always considered myself a pretty hard-assed soldier…mission, mission, mission,” said Lieutenant-Colonel Chris Linford, former commanding officer of the CF Health Services Clinic Pacific and executive officer of the combat hospital in Kandahar, who now lives in Victoria. But once, looking down at the body of a dead Canadian soldier, he found he’d changed. “I really began to doubt the mission. I began to feel…what is this cost we seem willing to pay?”
PTSD is not a cost paid by every soldier who serves or sees combat. Risk goes up with exposure to trauma, number of deployments and combat experience, but the majority of military personnel do not develop PTSD despite experiencing trauma or stress, being deployed or seeing combat. Through accumulated research the military is building a better sense of how many personnel sent to Afghanistan have been affected. A study of a random sample of the medical records of the personnel deployed between 2001 and 2008 showed that overall eight per cent had been diagnosed with mission-related PTSD and another 5.2 per cent with other mental health disorders, such as depression. A closer look at troops deployed from Gagetown in 2007 revealed the risk of PTSD goes up with combat exposure; about 20 per cent of them developed PTSD, and careers were cut short for half of those diagnosed.
For those who develop PTSD, the cost, therefore, can be high. As symptoms worsen, their lives begin to unravel. Insomnia, nightmares and flashbacks are common, and many handle this by drinking until their senses are deadened. “It became obvious if I drank enough I wouldn’t dream,” says a veteran of Afghanistan who lives on the West Coast. “I can completely understand how a lot of guys go off down that road.” For some, drinking bouts turn to addiction, adding a roadblock to recovery.
Isolation is also common. Some simply avoid people, places and activities that bring the trauma to mind, others are isolated by emotions like depression, guilt or worry. Some are constantly on alert, constantly feel stressed, on the brink of anger or tears. This maelstrom of symptoms can cost them their jobs, friendships and marriages, and damage relationships with their children. Some with persistent symptoms may never work again.
After Steve Dornan’s tour to Bosnia in 1995 he experienced quicksilver mood changes. “There was no decompression, there wasn’t even paperwork,” he said. “I literally just got off the plane, walked in (the house) and took off my uniform. You’re happy to be home; it’s over. It’s done.” But things did not get back to normal. “My daughter came in one day and said ‘I’m starving’ and I was literally screaming at her. I’d been dealing with kids that have no food, that have blown-off legs and arms, who’ve stepped on landmines, who’ve died in your arms, and she’s there healthy, safe and complaining.”
There were more over-the-top outbursts. “My wife said, ‘you have to do something; I won’t let you live like this with our family.’” So he approached his boss. “I said, ‘I’m not doing well at home.’ And he said, ‘There’s really nothing we can do here.’ A few weeks later, I was on my next tour,” said Dornan. “In the ’90s, that was their way of handling it.” He had flashbacks and was irritable and jumpy, but did not talk about it. “I put a lot of that in a little box in my head and put it away. It’s not something you talk about, it’s not something you can share, it’s not something people would understand.” He was finally diagnosed with PTSD in 2010 when he entered the care of Veterans Affairs Canada. He was medically released from the CF for an unrelated medical condition.
![[ILLUSTRATION: DAVID JUNKIN]](https://legionmagazine.com/wp-content/uploads/2013/03/PTSD3.jpg)
Bill Maguire was finally diagnosed with PTSD after he’d left the military following a 37-year career during which he managed to isolate himself both with his bristly personality and by working as much as he could. “I was a workaholic,” he said. “I had rage. I was very angry at everybody, always wanting to get into a fight, no respect for authority. I didn’t trust the high-ups, I think that was one of the big things, was trust, and I liked to throw temper tantrums.”
Things were no better at home. “I was having these horrendous nightmares.” He lashed out so often in his sleep that he and his wife had to sleep in separate bedrooms. The sound or sight of a dump truck would cause flashbacks to Cyprus, where the wounded and the dead bodies were carried out in large trucks. “Once I saw the wounded and dead in a big pile on top of each other. Cripes, what a mess, and blood running down the box, like hydraulic fluid. That’s one of the nightmares I have.”
The Canadian Forces has coined the term Operational Stress Injury (OSI) to describe the mental health problems—including depression, anxiety, PTSD—that can arise from the grim and exacting work of warriors and peacekeepers. Over the last decade diagnosis and treatment have become much more accessible. The Department of National Defence and Veterans Affairs Canada have developed a cross-country network of mental health clinics and Operational Trauma and Stress Support Centres. Support for military members, veterans and their families is available at Joint Personnel Support Units on bases and wings, through OSISS (the Operational Stress Injury Social Support program), and Military Family Resource Centres. The CF’s Road to Mental Readiness program reduces stigma by heightening awareness of symptoms, explaining what help is available, and encouraging people to seek treatment. It also provides resiliency training. “When awful things happen, people should react,” says Whelan. ‘It’s human to be horrified or distressed. Resiliency training gives them strategies to deal with that reaction—lets them know it’s OK to talk about it.”
These steps have reduced the stigma around seeking help, but haven’t eradicated individual reluctance. Members of the military are supposed to be tough, resilient, able to handle things on their own. “You don’t want to be that guy who puts his hand up and said he has a problem,” said Chris Dupee, a corporal who served in Afghanistan. “I’m an infantry guy. If you’ve got problems you drink it off, go party with the boys. You deal with your own problems.”
And once someone still serving does seek help, the wait for diagnosis can be agonizing. “From asking for help to diagnosis is like, six months,” said Dupee. “What happens between those two points can be very, very bad. And they’re not gonna get no leeway, no sympathy for their actions, because there is no diagnosis, there’s nothing to protect them. I know of a guy who went to jail within that time. And that’s bull crap.”
Waiting for diagnosis is isolating; so is treatment. And afterwards, so is living with PTSD. It’s part of the reason Dupee founded MilitaryMinds.ca, a website where people share their PTSD experiences. The website has many images of people holding up signs with the message: “We Are Not Alone.” Amassed, they present a powerful message. “There are a lot of people who say, ‘I’ve been watching (the website) the whole time and I’m finally ready to talk.’”
It can take years after symptoms develop for some to be ready to talk. Some, like the major known here as Philip, wanted to take care of duty first. Others, like Bill Maguire, didn’t know for decades what was wrong with them. And still others think they can handle it on their own. A young corporal, who wants to be known as John, was just back from Afghanistan when he heard a friend had just been killed on tour. “I started remembering everything that happened on my tour,” he said. Dangerous patrols, deaths, the wearing tension of constant vigilance. Two or three days later PTSD symptoms started: nightmares, flashbacks, depression. “I was reluctant to go for help because I thought I just needed time to myself.” Then he started thinking about suicide—and reached out. “They assigned me a social worker and psychologist right away.” He was given sleeping pills, anti-depressants, psychotherapy. Within six weeks the combination began to work.
“There is a moral imperative that when we put soldiers in combat, in harm’s way and they develop injuries, we’re going to treat them to the best of our abilities, with the best treatment available,” Major Paul Sedge, psychiatrist with the CF directorate of mental health in Ottawa, said at a forum in November. “We now have an economic argument that supports the moral imperative.” Over three years, the CF spent $1.2 million (nearly $18,000 each) treating the 67 Gagetown combat troops diagnosed with PTSD in the first year after they returned from their 2007 deployment. Each medical release is not only a loss of talent for the CF, but a loss of investment in skills and training—a quarter of a million dollars or more per serving member. Individuals lose their careers, some lose their ability to earn a living. VAC picks up responsibility for treatment if the veteran suffers from service-related PTSD after leaving the Forces. “There has been a steady increase in clients with PTSD over the past six years,” said psychologist Norman Shields, a researcher for the National Centre for Operational Stress Injuries at St. Anne’s Hospital near Montreal. As of September 2012, VAC had about 11,000 clients with PTSD who receive disability pensions or benefits under the New Veterans Charter for service-related injuries.
It’s in everybody’s interest that treatments work, and work well. And that is proven by research, which in the case of PTSD is still in relative infancy. “The mechanism involved (in developing PTSD) is not fully understood,” said Colonel Rakesh Jetly, adviser to the CF surgeon general on mental health and psychiatry. “But our understanding is becoming more sophisticated.” Current thinking is that something’s amiss with communication among the parts of the brain that govern fear response, filing and retrieving memories, and calming down.
When we sense danger, our brains go on high alert, assessing the danger and preparing the body to deal with it. Powerful stress hormones are released to ready the muscles to move, and quickly. The heart beats faster, blood vessels expand, blood pressure goes up, lungs expand. Nutrients are released from the liver, fat stores and bones to fuel muscle and brain. Lest there be wounds, blood vessels in the skin contract to limit bleeding and extra platelets are produced to speed blood clotting. In the blink of an eye, we’re ready to fight—or run—for our lives. If the situation isn’t dangerous after all, an all-clear signal is sent out and soothing hormones flood the brain, calming us down. We’ve only been startled. But after we come through a dangerous experience, the memory—and the strong emotions associated with it—is stored, so we can judge the danger and spring into action even faster next time.
In PTSD, this system goes awry. It’s thought some brain structures may be damaged by an overdose of stress hormones, the result of living with ever-present danger, like Corporal Dupee on daily patrol in Afghanistan. Or witnessing the daily horrors seen by Air Force veteran Dornan as he searched for mass graves in Bosnia. Or the steady increase in Peacock’s stress level from working long hours day after day, at a job where mistakes cost lives. Images of brains affected by PTSD have revealed a shrunken hippocampus—the area of the brain responsible for retrieving and storing memories—and a larger amygdala, which helps us learn to fear, or not fear, certain things. There is also a smaller volume of prefrontal cortex, the area responsible for dampening the stress response, calming the body down after danger or when in need to act despite danger, as in running out under fire to rescue a wounded comrade. As well, memories are not stored properly. If not stored as memory, the experience and its associated emotions are interpreted as current events by our brain’s early-warning system. A car backfiring may cause a person with PTSD to duck, run for cover or drag others to safety because that noise is associated with the emotion once felt under gunfire, an emotion the brain associates with danger. Each time that memory and emotion are called up, the link between them is strengthened. That’s why early treatment is important.
Although there are many different treatments for PTSD, there are only four so far that have been proven to work most of the time. They’re called “evidence-based” therapies, and favoured for use with military PTSD cases. Prolonged exposure therapy desensitizes people to PTSD’s overpowering emotions and addresses avoidant behaviour. Cognitive processing therapy addresses the effects of trauma on beliefs and thoughts. Eye Movement Desensitization and Reprocessing therapy helps with memory processing. Pharmacotherapy uses medications to control or alleviate symptoms.
The two psychotherapies—prolonged exposure and cognitive processing therapy—each reduce severity of symptoms by 60 to 80 per cent over a course of up to a dozen treatments, according to research presented at last November’s Military and Veterans Health Research Forum. However, they don’t work for every patient, and a quarter or more patients drop out of therapy because it involves repeatedly retelling and revisiting the traumatic event. Unpleasant side effects lead many to abandon drug therapy, too.
With effective treatment, the lives of those with PTSD are less painful. “There’s a scar, sure,” said Vancouver psychologist Dr. Marv Westwood. Poking that scar causes a reaction called “triggering”—a reawakening of symptoms. After treatment, people handle it better. “People know their triggers. They say, ‘Oh, I know where that is coming from; that’s why I had that response.’ They look around, recognize it’s safe, and move on.”
The reservist John found the treatments painful, but relief from the worst symptoms came relatively quickly. The first medications prescribed lessened insomnia, anxiety and depression. But they came with side effects.“The first four days were hell,” he said. “I had nausea, diarrhea, fever, blinding headaches, actual blindness where you see white lights, dizziness, everything. It’s pretty bad.” But he stuck with it and in six weeks, the drugs were working. Psychotherapy helped, too. “It’s kind of surreal,” he said. “It’s like someone is reading a story to you and it’s your story and it’s kind of weird. You break down more often because your body has to evacuate it from its brain. But then you start to feel better more often.” Exposure therapy worked on his intolerance of crowds so he was gradually able to take public transit to work in Toronto. It’s been two years now, and he hopes soon to be free of all therapy.
Bringing traumatic events to life in therapy sessions by describing sounds, the sights, colours and smells was painful and exhausting for Chris Linford. “I’d have to tell the same story three or four times. When the anxiety built [the therapist]…would have me actively apply the relaxation and breathing techniques. Over time…I seemed to be able to experience them and ride them through, and they wouldn’t affect me to nearly the same level.” His homework helped to slowly desensitize himself to triggers in his environment. The smell of blood or raw meat was such a big trigger that he couldn’t go into a grocery store. His wife Kathryn said it was a slow process involving repeated trips to the store during which he would walk closer and closer to the meat department. “Sometimes I’ll go into the store now and get out without even realizing I went into the meat section,” he said.
The medications and psychotherapy he received while in the CF relieved his symptoms, but he found a different kind of healing by stepping out into the community. “I was living a very isolated life,” he said. Military life is all about being part of a team, tackling and solving problems together, supporting and watching out for one another. “When you get sick with PTSD, for very good reasons, they extract you from that.” He has been posted away from his home unit to a Joint Personnel Support Unit during treatment. Personnel are posted to these units to receive medical treatment and rehabilitation and work assignments their home units aren’t equipped to provide. “But what they’ve also done is removed you from a lot of the support element that you used and counted upon throughout your career,” Linford said. He sampled a number of programs, including Outward Bound, Soldier On and the Veterans Transition Program, which bring veterans together for a group activity that provides emotional support while members simultaneously tackle tough personal PTSD issues. While they’re canoeing down a river, climbing a peak in the Himalayas or the Rockies, or learning new interpersonal skills, they also share their stories, their challenges, their successes, their insights with their peers. “I learned very quickly that I wasn’t alone,” he said. “That really gave me that nice feeling that you get in the centre of your chest when you’re part of . . . a team.”
Linford overcame this isolation by looking outward and there found support for looking inward. Military culture produces men and women who are stoic, knowing they might be wounded, injured or killed in the line of duty. They put others before self and mission and service to their country above all else. They strive to overcome all obstacles, to show no weakness. PTSD is a terrible wound for people with that expectation of strength and perfection. Consequently, military personnel are not good at asking for help. “They don’t like that feeling of…maybe a weakness, or a chink in the armour. I’d have put myself on that list,” said Linford. “I know I’m not cured; I’ll always have PTSD. But I recognize that identifying and accepting and being honest about my vulnerabilities led me to incredible strength. It’s funny that something that you’d assume would make you weak, actually makes you very strong. Once I figured that out, the doors started opening and my health started ratcheting up big time.”
One important insight is that recovery from PTSD is not a one-step process, and it can’t be accomplished alone. “There’s no magic blue pill,” said Linford. “It’s more like layering on.”
Therapy, medication, support of peers, family and community all have a role in healing. PTSD is everybody’s business. Members of the military need support of the civilian communities to which they return at the end of their military careers. But it’s not a one-way street. The community can also benefit from what the military has learned about preventing, treating and recovering from PTSD. “PTSD is not unique to the military,” said Jetly. “For us to sit and say the country has a moral obligation to help these young people who have gone and sacrificed, that will last for a couple of elections.” PTSD occurs in both the military and civilian community, he added. Research shows about 10 per cent of civilians develop PTSD at some point in their lives, the result of car crashes, fires, natural disasters, rapes, child abuse, beatings, shootings. That’s more than three million Canadian civilians who have struggled with insomnia, nightmares, flashbacks, numb emotions, quicksilver tempers, constant anxiety.
Civilians, too, cross the border into that foreign land, and have the same difficulty finding their way home. But family doctors are not as well informed about PTSD and how to treat it. Unlike in the military community, a civilian’s friends, neighbours and family are unlikely ever to attend a mental health education session. Stigma about mental health is still rampant in the civilian world. Jetly believes the military can help break down those barriers. The military program to reduce stigma can be used as a template for community programs, and research into best treatments for military personnel will ensure civilians also have treatments proven to be effective. And finally, said Jetly, military members with PTSD can talk about their experiences.
And so we come back to the nine men in that room in Halifax. A sense of duty may have compelled them to share their stories, so that there will be services—perhaps new and better ones—for this and future military generations wounded by PTSD. Each time veterans gather their courage to share their stories with the wider community, they increase the chances that this time, PTSD won’t be forgotten.
Email the writer at: sadams@legion.ca
Email a letter to the editor at: letters@legionmagazine.com
Advertisement