Ah, “sleep that knits up the ravelled sleeve of care”—a commodity that can be as elusive for injured and disabled Canadian Armed Forces personnel and veterans today as when Shakespeare penned the line 400 years ago to describe the insomnia of Macbeth, the soldier who killed his own king.
Insomnia and fatigue are common symptoms of physical and psychological injuries, like traumatic brain injury (TBI) from exposure to blast and post-traumatic stress and anxiety disorders. It’s also a symptom of some of the medications prescribed to treat those injuries. Unwanted sleepless nights are as old as the history of war.
Recent research in the United States has found that the risk of developing obstructive sleep apnea increases with the severity of PTSD. Aside from being the chief cause of stentorian snoring, sleep apnea can rouse a person hundreds of times a night, resulting in non-restful sleep and daytime fatigue.
“Veterans who come to PTSD treatment, even younger veterans, should be screened for obstructive sleep apnea, so they have the opportunity to be diagnosed and treated,” said researcher Sonya Norman, director of the PTSD Consultation Program at the National Center for PTSD in San Diego, California. Young veterans are less likely to be tested, she said. (Apnea is usually associated with age and being overweight.)
Diagnosis is important because untreated sleep apnea increases the risk for developing high blood pressure, diabetes and cardiovascular disease. It worsens symptoms of psychological injuries. Poor sleep quality makes serving personnel and veterans less resilient to stress and compromises their abilities to cope, according to research of the Durham VA (Veterans Administration) Medical Center at the University of North Carolina-Chapel Hill. A study of 2,597 veterans of Iraq and Afghanistan revealed nearly two thirds suffered poor sleep quality.
Further research is needed to better understand the impact of sleep quality on returning troops, and to help develop new ways to help veterans get better sleep, said VA research associate Jaime M. Hughes.
And research at the Military Suicide Research Consortium at Stanford University has linked poor sleep quality—insomnia, unrestful sleep and nightmares—to suicide.
Cognitive behavioural therapy, a prime treatment for PTSD, reduces suicidal thoughts when used to treat veterans with insomnia—independent of improvement in severity of depression. “Chronic insomnia is especially common among veterans,” said Dr. Timothy Morgenthaler, president of the American Academy of Sleep. “Effectively treating insomnia can be life-changing and potentially life-saving for veterans.”
The connection between service and sleep apnea is unclear, but disturbed sleep, prolonged sleep deprivation, fragmented sleep and hyperarousal are common in deployment and combat.
For some, add to that the chronic stress of PTSD.
In 2013, a study found obstructive sleep apnea is common after traumatic brain injury. One study showed about a third of civilians with TBI develop sleep-disordered breathing. A study of soldiers who served in Iraq and Afghanistan revealed a third had obstructive sleep apnea and more than half suffered insomnia. Insomnia plagued nearly two-thirds of those with blast injuries.
Only five per cent of Canadian personnel deployed to Afghanistan in 2009-10 reported TBI at their post-deployment screening, according to a report on the impact of the mission reported in 2014 by Mark Zamorski and David Boulos of the Canadian Forces Health Services Group in Ottawa. And most of those fell on the mildest end of the injury spectrum. Of those reporting problems, only a quarter had multiple persistent post-concussive symptoms, said the report.
However, the report pointed out that many seek mental health help years after deployment, pointing to the need for further research to shorten the time between development of symptoms and obtaining help.
Sometimes lifestyle changes like losing weight, avoiding alcohol and sleeping medications and stopping smoking alleviate sleep apnea.
Continuous Positive Airway Pressure (CPAP) therapy is the most effective non-surgical treatment. A CPAP machine increases air pressure in the throat during sleep so the airway doesn’t collapse. (There are reports it helps reduce nightmares, too). There are also dental devices that help keep the airway open. Surgery may be advised to correct a deviated nasal septum, remove soft tissue at the back of the throat or remove enlarged tonsils.
Some veterans with PTSD have trouble adjusting to CPAP, sleep medicine specialist Dr. Robert S. Rosenberg, of Prescott Valley, Arizona, said in an article in Everyday Health. “Although the airway opens immediately in response to treatment, it may take much longer for the limbic system and its stress response to return to normal.” Veterans report feeling claustrophobic and short of breath. But “if they stick with it, the majority will experience a real improvement in daytime symptoms,” he said.
Obstructive Sleep Apnea is on Veterans Affairs Canada’s table of disabilities, but years after leaving the Forces, it may be difficult for a veteran to prove the connection between apnea and military service. That’s one reason to be diagnosed while still in service, aside from the allure of better shut-eye. Another is that it improves the sleep quality of your partner (and depending on loudness of snoring, perhaps other members of the family, too).
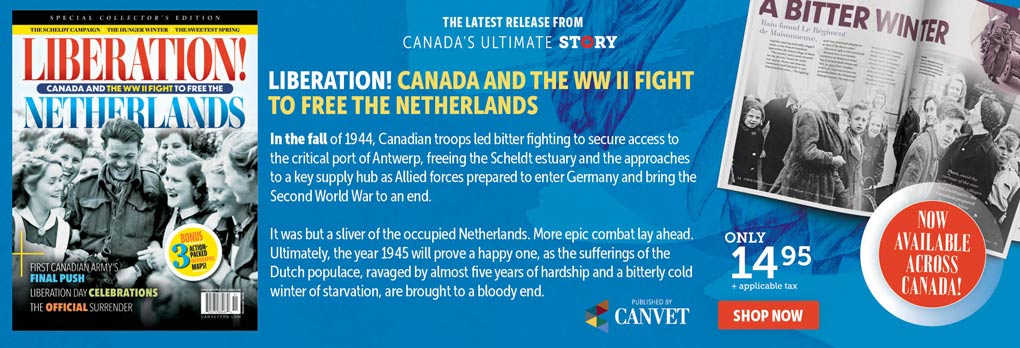
Advertisement