![BoomLead An IED blast rocks a Cougar, one of the armoured vehicles used by the Canadian Forces, in a test on the Suffield Experimental Proving Ground. [PHOTO: PHOTO GROUP, DRDC Suffield]](https://legionmagazine.com/wp-content/uploads/2011/10/BoomLead.jpg)
In 2008, Master Corporal Mike Trauner, deployed with the 3rd Battalion, Royal Canadian Regiment (3 RCR), was on foot patrol in the Zhari District west of Kandahar, Afghanistan, when a remotely controlled IED (improvised explosive device) was detonated under his feet. The blast blew off his legs and propelled him in a high arc six metres through the air. In 2010, on a road in the Panjwai District, a LAV III (light armoured vehicle) drove over a buried IED, setting off an explosion. The blast sent the 16,950-kilogram vehicle as much as a metre in the air and blew a hole in the bottom of the vehicle, breaking the bones in M.Cpl. Owen Kolasky’s feet and injuring his spine. In earlier wars, both likely would have died; today both soldiers hope to continue their Canadian Forces careers following rehabilitation.
Trauner and Kolasky are among dozens of Canadian military personnel who have survived blasts that would have proven fatal in 20th century military operations. They were saved by their armour and quick and effective life-saving battlefield treatment, both results of ongoing research dedicated to improving protection of Canadian Forces personnel from the many and evolving threats they face on ever-changing fields of battle.
“The armour of the vehicle is what actually allowed all of us to survive,” Kolasky, 25, said in an interview with Legion Magazine. He has seen the evolution of equipment between his first tour to Afghanistan in 2007 and his second in 2010. “The improvements that have been made in the vehicles…and that are continuing to be made are very specifically (geared) to the sorts of explosive threats we’re dealing with. I absolutely believe we (he and the four others in the LAV) survived due to the additional programs and armour.”
Blast injury has been described as the signature wound of the war in Afghanistan, claiming 97 of Canada’s 158 fallen soldiers, making amputees of dozens and wounding many others. It is the focus of programs at both Defence Research and Development Canada (DRDC) and the Canadian Forces to protect troops from being harmed by blasts, minimize blast injuries and improve treatment of blast injuries, including brain injury.“ It’s an enduring problem,” says Stephen Bjarnason, head of the casualty management section at DRDC Suffield in Alberta. “It’s been around ever since gunpowder was invented and somebody formed it into a bomb.” The end of Canada’s combat mission to Afghanistan has not ended the threat. “No matter where Canada goes in the world, IEDs are going to be a constant threat,” he says. “That’s the legacy of Afghanistan.”
Yet surprisingly, blast injury “is not as well understood as people thought it was,” says DRDC Suffield explosives expert Dr. John Anderson. Many questions remain—about the physics of blast, about the body’s response to blast, even how many Canadian troops have been exposed to blasts. Although concussions during deployment were reported by 116 (6.4 per cent) of 1,817 troops surveyed in 2009, nobody really knows the incidence of injury. Almost all Canadian troops in Afghanistan were in the vicinity of a blast sometime during deployment, but troops don’t report the exposure believing they were too far away to be affected and they feel no immediate symptoms, DRDC researcher Dr. Yushan Wang said at the Military and Veterans Research Forum in Kingston, Ont., a year ago. Yet the brain can be injured in a blast even when there are no physical symptoms, he added.
The CF releases reports on battle injuries once a year and does not release information about specific causes. The most recent report to the end of 2010 lists 615 wounded in action and 1,244 non-battle injuries in addition to those killed. It does say those listed as wounded in action include those injured from IEDs, mines, rocket attacks, combat and friendly fire as well as those who needed medical intervention for acute psychological trauma directly attributable to combat action. But there are no specific numbers about CF personnel killed or injured in blasts or how many have suffered blast brain injury. No one interviewed for this series wants terrorists to have any inkling of the results of their tactics.
Although great strides have been made in understanding what happens to the human body exposed to a blast and how to treat injuries, questions remain about the minimum blast level at which brain damage occurs, what happens with multiple low-level exposures, and long-term effects, including dementia in later life. It’s difficult to protect against an effect not yet measured.
![BoomInset1 M. Cpl. Owen Kolasky takes a break from loading a LAV III in Afghanistan, 2007. [PHOTO: OWEN KOLASKY]](https://legionmagazine.com/wp-content/uploads/2011/10/BoomInset1.jpg)
The best protection is avoidance of IEDs altogether, the idea behind the Canadian Forces Counter IED task force program, aimed at stopping bombers (Left of the Boom, January/February 2009). To the left of the boom, efforts are focused on choking off the supply of money to finance IEDs and supply of materials to make them, as well as catching and stopping the guys who make and plant the bombs. Meanwhile, efforts are also concentrated on increasing protection, minimizing injury and improving treatment of those that occur. The effort has produced remarkable medical advances—bandages that instantly stop bleeding; use of hypertonic saline solution to keep fluid levels up after massive blood loss, thus saving organs and limbs; improvements in use of tourniquets (Battle Tested Medicine, July/August 2008). Added to that are continuous improvements to body armour, vehicle armour and structure design. And now, a cutting-edge study at Suffield of blast damage at the molecular level has suggested the possibility of pharmaceutical prevention of some effects of blast injury to the brain.
But understanding how best to minimize blast injury must begin with an understanding of what happens during a blast. While a lot of data has been produced over the years by both physicists studying blast and medical researchers studying effects of blast, “they haven’t been talking that much to each other,” says Anderson. Some historical research used methods of testing that did not replicate a true blast from an IED or explosive attack, some did not take into account use of protective gear. “And there’s been extrapolations of injury to a human from injury that has occurred with animals—but nobody really understands the transfer function. Can you compare what happens to an animal directly to a human?”
This is but one question DRDC’s Blast Injury Program aims to answer. Established in 2009, the program is led by DRDC Suffield, though eventually researchers from five DRDC research centres across Canada, as well as universities, will be involved. Suffield provides a unique environment for researching such blast injury effects as brain injury, hemorrhage and crush injury because it is already home to the DRDC casualty management section and the military engineering section. Blast brain injury is a really complex problem,” says Bjarnason. “We found pretty well everywhere either people with medical know-how or people who knew how to blow things up. At Suffield we’ve got both of them in the same place. We’re in the ideal position to see how the two spheres overlap.”
Canadian Forces Base Suffield is located roughly 250 kilometres southeast of Calgary in the driest part of Alberta. At 2,690 square kilometres, it’s the largest Canadian Forces base and Commonwealth training facility in the world. DRDC Suffield takes up about 461 square kilometres of that area. Military research has been going on here for seven decades. Today DRDC Suffield is the lead laboratory for chemical and biological defence research, but also conducts research related to military engineering, mobility systems, and weapons system evaluation. Beginning in the 1960s, when the world was focused on effects of and protection from nuclear bombs, Suffield was a renowned centre for blast research. In 1961 news agencies reported that the biggest non-atomic explosion in history had occurred at Suffield, detonation of about 100 tons of TNT producing a mushroom cloud visible nearly 60 kilometres away and reports of atmospheric disturbances nearly 1,600 kilometres away in Michigan in the United States. More than 600 instruments were set up to record the explosion, producing data that would eventually be used for recommendations for building safer bomb shelters in the event of war, among other things.
A 50-metre long blast tube measuring 1.8 metres in diameter was built in the 1980s to produce and study controlled large blasts. But eventually other priorities took over, and the program “sort of ebbed away” as some researchers retired and others turned their attention to other threats, like protection from chemical and biological weapons, says Bjarnason.
However, the blast tube remains, and is expected to be refurbished within two years for use by the new blast injury program. With addition of a smaller blast tube, physicists will be able to consistently recreate shock waves that reflect what really happens during explosions of many sizes. “They’ll be able to create the same exposure conditions again and again and again,” says Bjarnason. Medical researchers using animal tissue will be able to study—right down to the molecular level—the effects of blast at various levels of pressure on various sorts of tissue and body systems.
![BoomInset2 You need land—lots of land—for testing explosives and protective equipment. Explosives expert Dr. John Anderson points to the wide open spaces at DRDC Suffield. [PHOTO: SHARON ADAMS]](https://legionmagazine.com/wp-content/uploads/2011/10/BoomInset2.jpg)
The program will “deliver operationally relevant information” to the Canadian Forces which has its own battle injury mitigation program, and Veterans Affairs Canada. Research data produced here could have implications for such military decisions as to how far apart troops should be spaced on patrol to where they should put their feet in an armoured vehicle to minimize injury to changes in design of body armour to better protect vital organs. It could help VAC determine effective support for the legions of CF personnel exposed to blasts in Afghanistan and other operations. And there will be a trickle-down effect to the civilian world as well, in such things as designing public spaces to minimize injury to civilians from terrorist attacks and suicide bombers.
But it all begins with understanding what happens during blasts such as those experienced by Trauner and Kolasky.
Ironically, Trauner says, it was lucky that the bomb he encountered, likely an artillery shell strapped to a mortar, was bigger than those troops normally encounter on foot patrol, and that the blast was set off when he was directly over it. If there had been less explosives or it had been detonated when he was a few feet away, he would not have been thrown in a high arc clear of the fireball and out of range of larger pieces of shrapnel capable of slashing through his body. “It would have blown me backwards and definitely could have made a mess of me.”
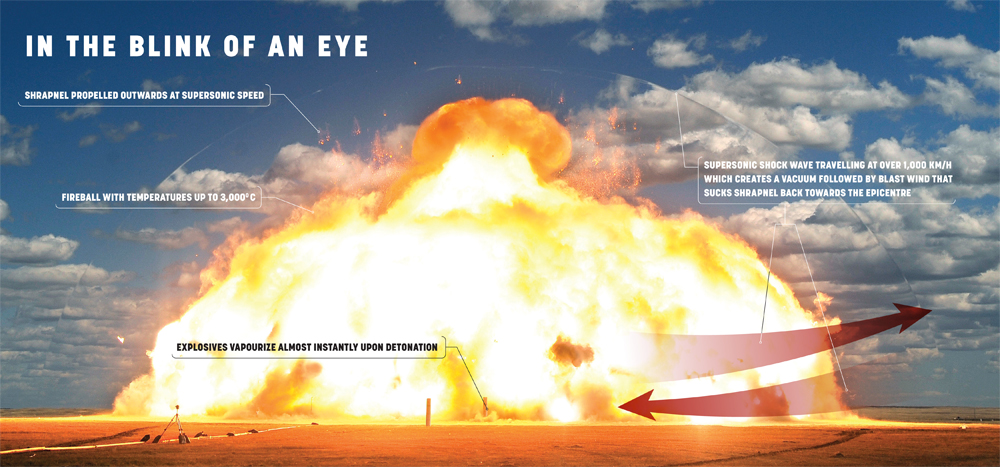
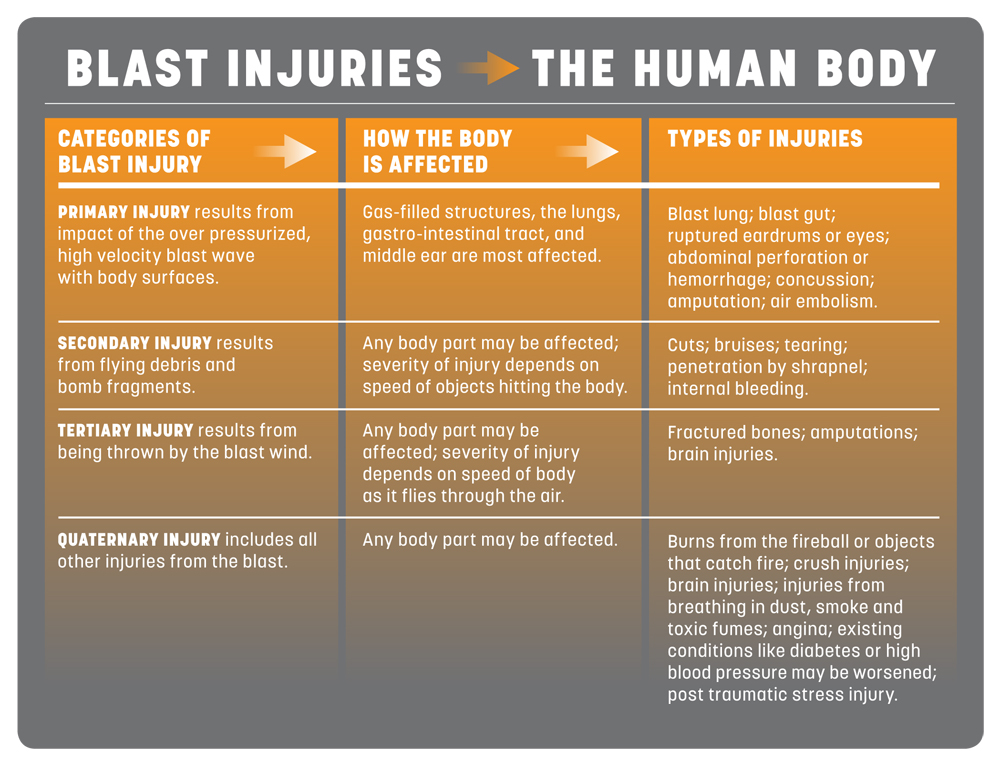
In detonations like those involving Trauner and Kolasky, the explosives are converted to hot gases almost instantaneously, creating a blast wave of super compressed air that travels out in all directions at supersonic speed, followed by a fireball that can reach 3,000 degrees Celsius and shrapnel. Air molecules are so compressed in the few millimetres of the blast front that the wave is like a solid object hurtling through space. The high pressure wave lasts only about a third of the time it takes to blink an eye, but delivers punishing blows as it passes.
This wave travels through the air, through bodies, around corners and over walls, its pressure amplified wherever it rebounds—between buildings, in corners of rooms or inside vehicles. Line of sight is required for injury by fragments in a ballistic attack, but in a blast “you could be hiding behind something and the blast wave will go over, around and through. It can go around corners. If you were hiding behind a wall it will go over and around and down and focus the pressure right on you,” says Anderson.
A large blast wave can propel a human body through the air and has enough force to rip off limbs, break bones and shear tissue. The blast wave is felt by those a distance away from the epicentre as a sudden thump in the chest. When the blast wave passes through a person it can rupture air-filled organs—eardrums, lungs, sinus, bowels. The eyes can be ruptured or damaged as thin surrounding bones are shattered. It can cause bubbles that block blood vessels in the brain or spinal cord. It can cause a catastrophic reduction in blood pressure and drop in heart rate. And it can damage brain tissue, but leave no symptoms at the time.
The explosion blows its container to smithereens, along with whatever else malevolent bomb makers have tucked inside, creating shrapnel that is swept along behind the blast wave. Fragments from the bomb and flying debris demolish windows, shred wood, pulverize plastic, break brick and stone to produce glass shards, wood splinters and shrapnel travelling faster than hurricane winds. As the primary blast wave moves out from the centre of the explosion, a vacuum is created and air rushes in, sucking debris at high speed back in the other direction. Humans caught in such an onslaught suffer deep cuts and crushing injuries as they are thrown against the ground or nearby vehicles and structures and airborne objects fly through them or land on top of them. Then follows injury from the heat and noxious chemicals generated by the explosion—burns from the blast itself or from things in the environment set alight, respiratory injuries from breathing in super-heated air, smoke and particulates. Unprotected people caught in the primary blast radius of a high order explosive, who get the full force of pressure changes, heat and shrapnel, are likely to die.
But Trauner and Kolasky were not unprotected. Trauner was protected by blast armour—a helmet, special eyewear, plated body armour, blast gloves; Kolasky was wearing body armour and was in an armoured vehicle. Teams of specialists at DRDC and with the CF are dedicated to the continual redesign of equipment, the culmination of a decade’s worth of research in Canada’s experience in Afghanistan, to give Canadian troops the best possible chance of surviving blasts and minimizing injuries from them.
Email the writer at: writer@legionmagazine.com
Email a letter to the editor at: letters@legionmagazine.com
Advertisement